From a biochemical standpoint detoxification can be described as the metabolic process by which a series of enzymatic reactions neutralise and solubilise exogenous and endogenous toxins for transport and excretion from the body. This is achieved through the well described system known as Phase I and Phase II detoxification pathways.
Phase I is typically composed mainly of the cytochrome P450 supergene family of enzymes, begins the detoxification process by chemically transforming lipid soluble compounds into intermediate metabolites in preparation for Phase II detoxification.
In Phase II reactions the intermediate metabolites produced in Phase I are transformed into water-soluble compounds that can be excreted through urine or bile. This involves several types of nutrient dependant reactions, including glucuronidation, sulfation, glycination, glutathionation and amino acid conjugation.
Most literature on detoxification refers to these two phases, with greater emphasis traditionally placed on Phase I. The liver has long been recognised as the primary organ of detoxification but, there is now growing evidence that the gut also plays a central role in the detoxification process. Given that the small intestine functions predominantly as an absorptive organ its significance in the metabolism of non-nutritive dietary constituents and xenobiotics seems to have been significantly underestimated. This is in spite of the fact that the small intestine is the first site of xenobiotic exposure and that, over the course of a lifetime, is presented with the largest load of antigens and xenobiotics confronting the human body.
THE ANTIPORTER SYSTEM
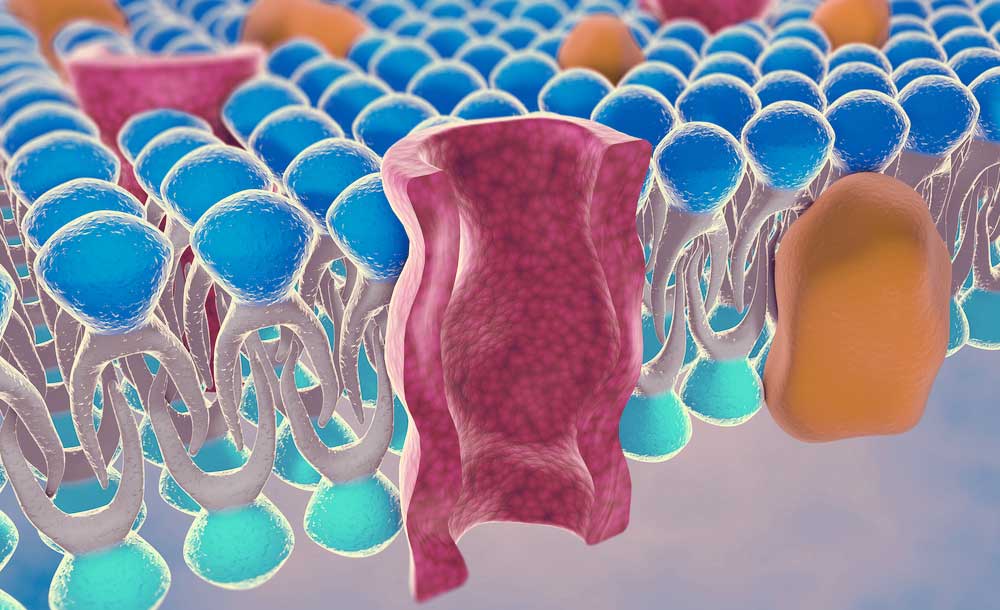
Emerging evidence is now describing an additional detoxification process which is highly concentrated in the small intestine, known as antiporter activity. This is now often referred to as the Phase III detoxification system.[1] More than 350 unique antiporter proteins have been identified with the best known and most studied transporter known as P-glycoprotein. These efflux transporters, like Phase I and Phase II enzymes, work on specific substrates. Efflux transporters can also be induced, increasing the transporters activity. They can also be inhibited causing substrate levels to become higher.
P-glycoprotein is extensively distributed and expressed in the intestinal epithelium where it pumps xenobiotics back into the intestinal lumen. It is also found in liver cells where it pumps toxins into bile ducts, in the cells of the proximal tubule of the kidney where it pumps them into urine-conducting ducts, and in the capillary endothelial cells composing the blood–brain barrier and blood-testis barrier, where it pumps them back into the capillaries.[2]
Antiporter activity is an important factor in the first-pass metabolism of xenobiotics, thereby decreasing the intracellular concentration of xenobiotics and reducing total toxin load in the liver.[3] This energy-dependent trans-membrane protein has also been associated with the Phase I enzyme CYP3A which appears to play a role in the co-regulation of this system in the intestines to further promote detoxification.[4]
In the small intestine, antiporter activity is found at the tips of the villi [5] and by pumping non-metabolised xenobiotics out of cells and back into the intestinal lumen may reduce the total load on Phase I and allow for greater xenobiotic detoxification efficiency before metabolised toxins are transported into the circulation.
PHASE III DETOXIFICATION
While the antiporter system is described primarily through its role in first-pass metabolism, occurring pre-Phase I and Phase II, the same efflux pump is also responsible for the transport of hydrophilic metabolites out of hepatocytes after Phase II conjugation, and is therefore referred to as Phase III of detoxification. Thus, the antiporter system serves a dual function with the Phase III terminology used to describe both functions of transportation of conjugated metabolites after Phase II and the elimination of toxins pre-biotransformation.
WASTE REMOVAL
Conjugated xenobiotics and toxins are pumped into the bile and intestinal lumen by the antiporter system so they can be excreted. At this stage, effective elimination of these compounds is dependant on a number of factors, with diet and microflora playing a pivotal role. Deconjugation of these metabolites by hydrolytic enzymes such as beta-glucuronidase, sulfatase and beta-lyase results in subsequent enterohepatic recirculation, shunting the toxin back to the liver where it will, once again, go through the biotransformation process.
Resident bacteria in the GI tract are largely responsible for the production of these enzymes, with beta-glucuronidase recognised as particularly significant, being present throughout the GI tract, due to the fact that glucuronides are the largest class of xenobiotic conjugates excreted in the bile.[6] This process is attributed to enzyme activity produced significantly by Clostridium perfringens as well as Escherichia coli and Klebsiella sp.,[7] suggesting that dysbiosis may contribute to increased metabolite deconjugation and enterohepatic recirculation. Elevated beta-glucuronidase activity is associated with an increased risk for various cancers, particularly hormone-dependent cancers such as breast, prostate, and colon cancers.[8]
The implications of this further support the notion that diet and probiotic supplementation may assist with normal detoxification processes. In addition, calcium d-glucurate, a nutrient found in grapefruit, apples, oranges, broccoli, and brussels sprouts is known to be a beta-glucuronidase inhibitor via its metabolite D-glucaro-1,4-lactone. Oral supplementation of calcium-D-glucarate has also been shown to inhibit beta-glucuronidase activity [9] resulting in the proper elimination of conjugated toxins.
According to Dr Chris Shade, an environmental and analytical chemist who specialises in the human detoxification system, the most significant cause of Phase III dysfunction is inflammation, especially in the gut. When Phase III is blocked a negative feedback loop results in the down regulation of Phase II enzymes. Intermediate metabolites produced in Phase I are then at risk of building up resulting in increased oxidative damage which further impairs detoxification capacity.[10]
The clinical goal here should include supporting the GI tract by reducing inflammation, binding toxins in the gut and promoting efficient elimination. Therapeutic considerations may include high-bioavailability curcumin, chlorella and water soluble fibre. Consider also supplementing with nutrients required for normal Phase II function and antioxidant support which specifically includes glutathione and R-alpha-lipoic acid. These nutrients have poor bioavailability and would therefore have limited therapeutic value unless provided in a more advanced delivery system. Liposomal technology allows these nutrients to be delivered in nano-sized vesicles for enhanced absorption through the mucosa of the mouth.
The human detoxification system is a delicate and complex process involving three distinct phases. However, it is only very recently that we have elucidated the function and significance of Phase III. We now understand that any successful therapeutic management of detoxification requires us to restore, manage and augment this phase, which can then have profound implications for health and resilience.
REFERENCES
- Liska DJ. The detoxification enzyme systems. Alt Med Rev 1998;3(3):187-198. [PDF]
- Ueda K, Clark DP, Chen CJ,et al. (The human multidrug resistance (mdr1) gene. cDNA cloning and transcription initiation. J Biol Chem 1987;262(2):505-508. [Full Text]
- Chin KV, Pastan I, Gottesman MM. Function and regulation of the multidrug resistance gene. Adv Cancer Res 1993;60:157-180. [Abstract]
- Wacher VJ, Wu CY, Benet LZ. Overlapping substrate specificities and tissue distribution of cytochrome P450 3A and P-glycoprotein: Implications for drug delivery and activity in cancer chemotherapy. Mol Carcinog 1995;13:129-134. [Full Text]
- Carey WD. Current Clinical Medicine, 2nd Ed. Philidelphia: Elsevier, 2010.
- Rowland IR (Ed). Role of the gut flora in toxicity and cancer. London: Academic Press, 1988.
- Leung JW, Liu YL, Leung PS, et al. Expression of bacterial beta-glucuronidase in human bile: an in vitro study. Gastrointest Endosc 2001;54(3):346-350. [Abstract]
- Walaszek Z, Szemraj J, Narog M, et al. Metabolism, uptake, and excretion of a D-glucaric acid salt and its potential use in cancer prevention. Cancer Detect Prev 1997;21:178-190. [Abstract]
- Calcium-D-glucarate Monograph. Altern Med Rev 2002;7(4):336-339.[Full Text]
- Shade C. Mercury and the human detoxification system. Quicksilver Scientific, LLC Lafayette. (11-Sept-2010) [Full Text]
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.