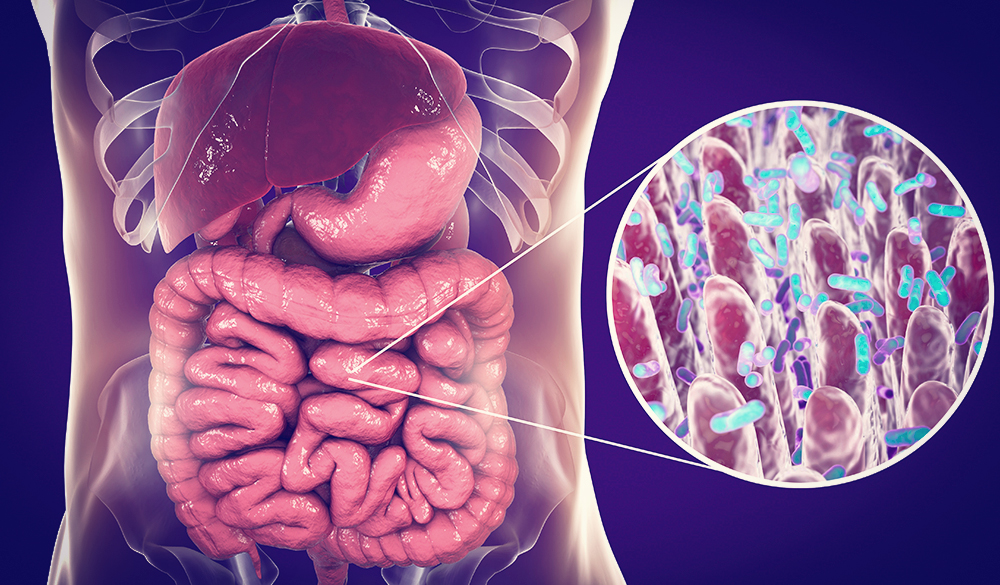
The intestinal microbiome is a complex signalling hub that incorporates environmental factors, such as diet, stress and xenobiotics, with genetics and immune signals to influence host immunity and response to infection.[1-3] Within the last decade, we have begun to understand the importance of this interdependent bilateral interaction between the host and its microbiota and how its mutually beneficial balance is crucial in host defence and immune health.[1]
Dysbiosis, the term used to describe commensal microbial imbalance, plays a role in the pathogenesis of common gastrointestinal tract (GIT) complaints and acute upper respiratory tract infections (URTIs).[4] It is also considered a causative factor in extraintestinal inflammatory and autoimmune disorders such as inflammatory bowel disease, and is suspected to contribute to the progression of pulmonary disease and atopic conditions.[1,2] The mechanisms that are involved in the crosstalk between the microbiome and our immune system need to be tightly controlled, in order to avoid the aberrations that contribute to the aetiology of common multifactorial disorders.[1]
One way in which to help influence a positive benefit for immunity host-microbiome mutualism, is to support microbial balance via certain probiotic strains. Saccharomyces boulardii (SB), Lactobacillus acidophilus, L. casei, L. plantarum, L. rhamnosus, Bifidobacterium bifidum, B. breve, B. longum, B. lactis and Streptococcus thermophilus have shown to help either balance disturbed intestinal microflora, the related dysfunction of the GIT, and in turn, positive support for immune function and health.[6-11]
A daily intake of B. bifidum and B. infantis has demonstrated a reduction in the frequency of cold and flu during periods of acute stress for undergraduate students.[3] L. acidophilus and L. casei have been shown to adhere to the intestinal mucosa and may block the adherence of enteropathogens which threaten immune health.[12] L. plantarum is most often associated with antimicrobial bacteriocin production, which reduces the survival of competing pathogens.[12]
SB is an extensively researched antibiotic-resistant strain of yeast that has shown probiotic effects through maintaining healthy gastrointestinal immunity, with particular relevance for antibiotic-associated diarrhoea, recurrent Clostridium difficile intestinal infections,[13] Candida albicans attachment-inhibition and reduction of pro-inflammatory mediators in the digestive system.[14]
In the urogenital tract, lactobacilli species such as L. rhamnosus, help to maintain healthy immunity by reducing the overgrowth of less desirable species,[15] working synergistically with various proteins that protect the host from pathogens, including lactoferrin.[16]
As our bodies are inhabited by a large number of microorganisms that reside on various surfaces including the skin, gastrointestinal, respiratory and urogenital tracts, it is essential to help cultivate a symbiotic relationship that benefits whole-organism physiology and immune health.
References
- Thaiss CA, Zmora N, Levy M, et al. The microbiome and innate immunity. Nature 2016;535(7610):65-74. [Abstract]
- Petersen C, Round JL. Defining dysbiosis and its influence on host immunity and disease. Microreview 2014;16(7):1024-1033.[Abstract]
- Langkamp-Henken B, Rowe CC, Ford AL, et al. Bifidobacterium bifidum R0071 results in a greater proportion of healthy days and a lower percentage of academically stressed students reporting a day of cold/flu: a randomised, double-blind, placebo-controlled study. Br J Nutr 2015;113(3):426-434.[Abstract]
- King S, Glanville J, Sanders ME, et al. Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysis. Br J Nutr 2014;112(1):41-54. [Abstract]
- Bibbo S, Ianiro G, Dore MP, et al. Gut microbiota as a driver of inflammation in non-alcoholic fatty liver disease. Mediators Inflamm 2018; 2018:9321643.[Full Text]
- Kailasapathy K, Chin J. Survival and therapeutic potential of probiotic organisms with reference to Lactobacillus acidophilus and Bifidobacterium spp. Immunol Cell Biol 2000;78(1):80-88.[Abstract]
- Correa NB, Peret Filho LA, Penna FJ, et al. A randomized formula controlled trial of Bifidobacterium lactis and Streptococcus thermophiles for prevention of antibiotic-associated diarrhea in infants. J Clin Gastroenterol 2005;39(5):385-389.[Abstract]
- Tien MT, Girardin SE, Regnault B, et al. J Immunol 2006;176(2):1228-1237. [Abstract]
- Hessle C, Hanson LA, Wold AE. Clin Exp Immunol 1999;116(2):276-282. [Abstract]
- Yasui H, Shida K, Matsuzaki T, et al. Antonie Van Leeuwenhoek 1999;76(1-4):383-389. [Abstract]
- Thibault H, Aubert-Jacquin C, Goulet O. J Pediatr Gastroenterol Nutr 2004;39(2):147-152. [Abstract]
- Fooks LJ, Gibson, GR. Probiotics as modulators of the gut flora. Br J Nutr 2002;88(Suppl 1):S39-49.[Abstract]
- Czerucka D, Piche T, Rampal P. Review article: yeast as probiotics – Saccharomyces boulardii. Aliment Pharmacol Ther 2007;26(6):767-778.[Abstract]
- McFarland LV. Systematic review and meta-analysis of Saccharomyces boulardii in adult patients. World J Gastroenterol 2010;16(18):2202-2222.[Abstract]
- Pizzorno JE Jr, Murray MT (Eds), Textbook of natural medicine, 3rd ed. (pp.2155-2165). St Louis: Churchill Livingstone Elsevier, 2006.[Source]
- Valenti P, Rosa L, Capobianco D, et al. Role of lactobacilli and lactoferrin in the mucosal cervicovaginal defense. Front Immunol 2018;9:376.[Full Text]
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.