Inflammation is a defence mechanism initiated by the body’s immune system in response to perceived harmful stimuli such as trauma, infection and/or auto-immune disease.1 The purpose of inflammation is to initiate healing, making it crucial to both recovery and repair.
While acute inflammation is protective, low-grade systemic inflammation that is chronic, has been identified as a causal factor of many chronic diseases; in fact, more than half of all deaths are attributable to inflammation related diseases, these include cardiovascular disease, type 2 diabetes mellitus, autoimmune and neurodegenerative conditions.2
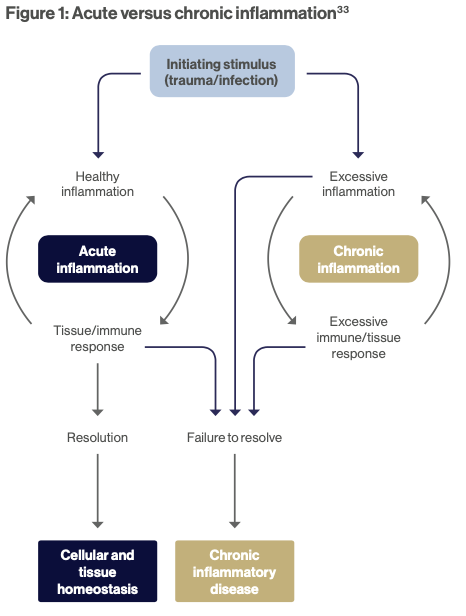
Acute versus chronic inflammation
Inflammatory challenges are encountered daily, however timely resolution of the acute inflammatory process is often under appreciated due to the innate ability of the body to repair. Inflammation that is acute typically starts rapidly and in response to injury. Inflammatory pathways are activated by the immune system leading to the release of cytokines as well as eicosanoids such as prostaglandins and leukotrienes derived from arachidonic acid. The recruitment of large numbers of leucocytes with neutrophils mediate inflammation and promote tissue repair. (See Figure 1)
Acute inflammation that is uncontrolled and unresolved becomes chronic, often lasting for prolonged periods of several months to years.
In chronic conditions, inflammation and repair occur concurrently, rather than consecutively, due to constant exposure to the irritant. Fibrosis and granuloma formation occur in combination with the destruction of tissue architecture. The dominant, infiltrating cell being the macrophage which functions to remove apoptotic neutrophils3 and restore homeostasis.
Resolution of inflammation versus reducing inflammation
When working with chronic inflammation in clinical practice, the focus has typically been on reducing inflammation, however, re-examining chronic inflammatory diseases through the lens of failed or dysregulated resolution is crucial to assist with resolution of inflammation.17
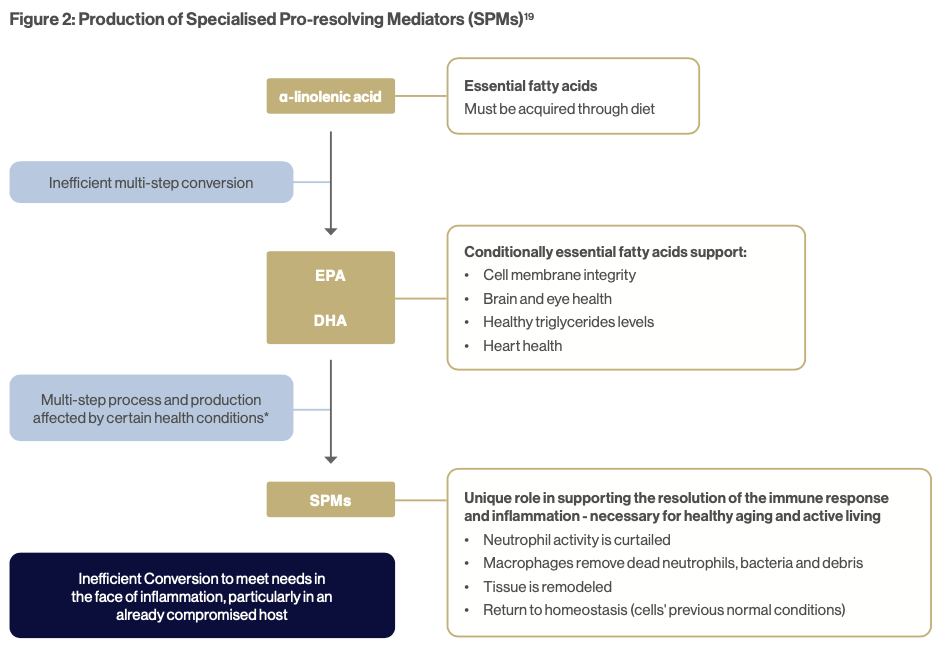
SPMs are molecules that are derived endogenously from arachidonic acid, docosapentaenoic acid (DPA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) and are produced to counterbalance inflammatory cues.18 Unlike conventional anti- inflammatories, SPMs not only work by blocking the inflammatory process, but also by reprogramming immune cells and enhancing leukocyte efferocytosis, thus assisting with terminating and resolving the inflammatory process.19 (See Figure 2).
The turning point in the transition from an inflammatory to a non-inflammatory state is a switch in the synthesis of lipid mediators from pro-inflammatory lipid mediators to the synthesis of specialised pro-resolving mediators (SPM’s) during the acute inflammatory phase.18
When reducing inflammation does not work
While the switch from an inflammatory to a non-inflammatory state has been shown to occur in healthy individuals, it may not occur in individuals with a chronic inflammatory condition or dysbiosis.20 The pathways involved with the synthesis of SPMs from omega-3 fatty acids are impaired. In these individuals, a focus on reducing inflammation rather than resolving inflammation may be ineffective.
Barden et al. (2019)21 observed that individuals with metabolic syndrome and obesity demonstrated dysregulated inflammatory pathways, preventing them from making adequate SPMs required to resolve inflammation. This was remedied with weight loss and improving insulin sensitivity.
Holistic treatment of inflammation
Green space
Immersion in nature is associated with a more favourable inflammatory profile. Serum levels of interleukin-8 (IL-8) and TNF-α were significantly decreased after 2 hours of exposure to a forest environment in stressed young adults compared to placebo.22 This is hypothesised to be due in part to exposure to anti-inflammatory terpenes released from trees which block the inflammatory cascade.23
Sauna
An inverse, dose–response relationship has been found between regular use of sauna and reduced levels of CRP.24 Acute exposure to heat increases IL-6, triggering the release of interleukin-10 (IL-10), inhibiting several pro-inflammatory cytokines.25
Connection
Relationships that are characterised by connection and support are associated with lower levels of systemic inflammation compared to individuals who experience unsupportive or hostile relationships.26 Higher levels of IL-6 & TNF-a were observed in couples experiencing sustained marital conflict.27
Movement & stretching
Both exercise and stretching have been shown to assist with the resolution of acute inflammation by enhancing the production of SPMs and promoting macrophage phagocytosis in vivo.28,29
Diet
Dietary patterns that emphasise a whole food diet such as the Mediterranean diet are associated with lower levels of inflammatory cytokines, CRP and TNF-α.30 Key components include; seasonal fruits and vegetables, herbs & spices, anti-inflammatory fats such as extra virgin olive oil31 as well as omega-3 rich fish.
Supplementation
Targeting both reducing inflammation and resolving inflammation would appear most efficacious when managing chronic inflammatory conditions. In an open-label pilot study, involving 29 individuals with inflammation-associated discomfort, consumption of a combined SPM-enriched marine oil and curcumin supplement taken daily for 60 days resulted in a significant reduction in pain.32
Working with patients to identify triggers for both acute and chronic inflammation, and addressing the root cause of inflammation is key to reducing inflammation. For those patients already in a state of chronic inflammation, enhancing SPM levels both endogenously and exogenously supports the reduction in ongoing inflammation and is supported by dietary and lifestyle changes, where needed. Supporting patients through the supplementation of SPMs can accelerate this process and should be considered a first-line treatment for chronic inflammation.
DOWNLOAD A PDF VERSION OF THIS ARTICLE
References
1. Feehan KT, Gilroy DW. Is Resolution the End of Inflammation? Trends Mol Med. 2019 Mar;25(3):198-214. doi: 10.1016/j.molmed.2019.01.006
2. Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019 Dec;25(12):1822-1832. doi: 10.1038/s41591-019-0675-0.
3. Pahwa R, Goyal A, Jialal I. Chronic Inflammation. 2022 Aug 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29630225.
4. Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and met- abolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021 Mar 1;320(3):C375-C391. doi: 10.1152/ajpcell.00379.2020. Epub 2020 Dec 23. PMID: 33356944
5. Henson J, Yates T, Edwardson CL, Khunti K, Talbot D, Gray LJ, Leigh TM, Carter P, Davies MJ. Sedentary time and markers of chronic low-grade inflammation in a high risk population. PLoS One. 2013 Oct 29;8(10):e78350. doi: 10.1371/journal.pone.0078350
6. Twardowska A, Makaro A, Binienda A, Fichna J, Salaga M. Prevent- ing Bacterial Translocation in Patients with Leaky Gut Syndrome: Nutrition and Pharmacological Treatment Options. Int J Mol Sci. 2022 Mar 16;23(6):3204. doi: 10.3390/ijms23063204.
7. Ricker MA, Haas WC. Anti-Inflammatory Diet in Clinical Prac- tice: A Review. Nutr Clin Pract. 2017 Jun;32(3):318-325. doi: 10.1177/0884533617700353. Epub 2017 Mar 28. PMID: 28350517.
8. Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nature Rev Immunol. 2011;11:625–32.
9. Muscatell KA, Inagaki TK. Beyond social withdrawal: New per- spectives on the effects of inflammation on social behavior. Brain Behav Immun Health. 2021 Jul 27;16:100302. doi: 10.1016/j. bbih.2021.100302.
10. Irwin MR, Olmstead R, Carroll JE. Sleep Disturbance, Sleep Dura- tion, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol Psychiatry. 2016 Jul 1;80(1):40-52. doi: 10.1016/j.biopsych.2015.05.014.
11. Ganey PE, Roth RA. Concurrent inflammation as a determinant of susceptibility to toxicity from xenobiotic agents. Toxicology. 2001 Dec 28;169(3):195-208. doi: 10.1016/s0300-483x(01)00523-6. PMID: 11718960.
12. Abdelsalam NA, Ramadan AT, ElRakaiby MT, Aziz RK. Toxicomicro- biomics: The Human Microbiome vs. Pharmaceutical, Dietary, and Environmental Xenobiotics. Front Pharmacol. 2020 Apr 16;11:390. doi: 10.3389/fphar.2020.00390. PMID: 32372951.
13. D’Elia ATD, Juruena MF, Coimbra BM, Mello MF, Mello AF. Increased immuno-inflammatory mediators in women with post-traumatic stress disorder after sexual assault: 1-Year follow-up. J Psychiatr Res. 2022 Nov;155:241-251. doi: 10.1016/j.jpsychires.2022.08.028
14. Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis fac- tor-α. Mol Psychiatry. 2016 May;21(5):642-9. doi: 10.1038/mp.2015.67. Epub 2015 Jun 2. PMID: 26033244; PMCID: PMC4564950.
15. Leschak CJ, Eisenberger NI. Two Distinct Immune Pathways Linking Social Relationships With Health: Inflammatory and An- tiviral Processes. Psychosom Med. 2019 Oct;81(8):711-719. doi: 10.1097/PSY.0000000000000685. PMID: 31600173; PMCID: PMC7025456.
16. Cole SW, Levine ME, Arevalo JM, Ma J, Weir DR, Crimmins EM. Lone- liness, eudaimonia, and the human conserved transcriptional response to adversity. Psychoneuroendocrinology 2015;62:11–7.
17. Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019 Dec;25(12):1822-1832. doi: 10.1038/s41591-019-0675-0.
18. Julliard WA, Myo YPA, Perelas A, Jackson PD, Thatcher TH, Sime PJ. Specialized pro-resolving mediators as modulators of immune responses. Semin Immunol. 2022 Jan;59:101605. doi: 10.1016/j. smim.2022.101605. Epub 2022 Jun 2. PMID: 35660338.
19. Serhan CN. Pro-resolving lipid mediators are leads for resolution physiology. Nature. 2014 Jun 5;510(7503):92-101. doi: 10.1038/na- ture13479. PMID: 24899309.
20. Norris, P.C.; Skulas-Ray, A.C.; Riley, I.; Richter, C.K.; Kris-Etherton, P.M.; Jensen, G.L.; Serhan, C.N.; Maddipati, K.R. Identification of specialized pro-resolving mediator clusters from healthy adults after intravenous low-dose endotoxin and omega-3 supplementation: A methodological validation. Sci. Rep. 2018, 8, 18050
21. Barden A, Shinde S, Tsai IJ, Croft KD, Beilin LJ, Puddey IB, Mori TA. Effect of weight loss on neutrophil resolvins in the metabol- ic syndrome. Prostaglandins Leukot Essent Fatty Acids. 2019 Sep;148:25-29. doi: 10.1016/j.plefa.2019.07.001. Epub 2019 Jul 3. PMID: 31492430.
22. Im S.G., Choi H., Jeon Y.-H., Song M.-K., Kim W., Woo J. M. Compari- son of effect of two-hour exposure to forest and urban environments on cytokine, anti-oxidant, and stress levels in young adults. Int. J. En- viron. Res. Public Health. 2016;13:625. doi: 10.3390/ijerph13070625.
23. Andersen L, Corazon SSS, Stigsdotter UKK. Nature Exposure and Its Effects on Immune System Functioning: A Systematic Review. Int J Environ Res Public Health. 2021 Feb 3;18(4):1416. doi: 10.3390/ ijerph18041416. PMID: 33546397
24. Laukkanen J.A., Laukkanen T. Sauna bathing and systemic inflammation. Eur. J. Epidemiol. 2017;33:351–353. doi: 10.1007/ s10654-017-0335-y
25. Henderson KN, Killen LG, O’Neal EK, Waldman HS. The Car- diometabolic Health Benefits of Sauna Exposure in Individuals with High-Stress Occupations. A Mechanistic Review. Int J Environ Res Public Health. 2021 Jan 27;18(3):1105. doi: 10.3390/ijerph18031105. PMID: 33513711
26. Fairbank EJ, McGrath JJ, Henderson M, O’Loughlin J, Paradis G. So- cial support and C-reactive protein in a Québec population cohort of children and adolescents. PLoS One. 2022 Jun 22;17(6):e0268210. doi: 10.1371/journal.pone.0268210. PMID: 35731783
27. Fagundes CP, Bennett JM, Derry HM, Kiecolt-Glaser JK. Relationships and Inflammation across the Lifespan: Social Devel- opmental Pathways to Disease. Soc Personal Psychol Compass. 2011 Nov;5(11):891-903. doi: 10.1111/j.1751-9004.2011.00392.x
28. Berrueta L, Muskaj I, Olenich S, Butler T, Badger GJ, Colas RA, Spite M, Serhan CN, Langevin HM. Stretching Impacts Inflammation Res- olution in Connective Tissue. J Cell Physiol. 2016 Jul;231(7):1621-7. doi: 10.1002/jcp.25263
29. Calderin EP, Zheng JJ, Boyd NL, McNally L, Audam TN, Lorkiewicz P, Hill BG, Hellmann J. Exercise-induced specialized proresolving me- diators stimulate AMPK phosphorylation to promote mitochondrial respiration in macrophages. Mol Metab. 2022 Dec;66:101637. doi: 10.1016/j.molmet.2022.101637
30. Mukherjee MS, Han CY, Sukumaran S, Delaney CL, Miller MD. Effect of anti-inflammatory diets on inflammation markers in adult human populations: a systematic review of randomized controlled trials. Nutr Rev. 2022 Dec 6;81(1):55-74. doi: 10.1093/nutrit/nuac045
31. Schwingshackl L, Christoph M, Hoffmann G. Effects of Olive Oil on Markers of Inflammation and Endothelial Function-A Systematic Review and Meta-Analysis. Nutrients. 2015 Sep 11;7(9):7651-75. doi: 10.3390/nu7095356.
32. Jaja-Chimedza, A., Hirsh, S., Bruce, D. et al. The effects of an SPM-enriched marine oil and bioavailable curcumin combination on inflammation-associated discomfort in generally healthy individuals: a virtual open-label pilot study. Translational Medicine Communica- tions 7, 25 (2022). https://doi.org/10.1186/s41231-022-00131-7
33. Anderton, H., Wicks, I.P. & Silke, J. Cell death in chronic inflammation: breaking the cycle to treat rheumatic disease. Nat Rev Rheumatol 16, 496–513 (2020). https://doi.org/10.1038/s41584-020-0455-8