Complementary health practitioners have a critical role in the wellness of people diagnosed with cancer. Patients know this! About half of those diagnosed with cancer are not satisfied with the choices offered by conventional medicine and initiate the use of complementary care.[1] In a New Zealand regional cancer treatment centre, 49% of patients used complementary care including vitamins, antioxidants, specific diets, and herbal therapies.[2] Most of these people used complementary therapies to improve the quality of life and one third used these therapies with the hopes of curing cancer. While two thirds of these patients felt that the complementary therapies were helpful, only 41% discussed their use with their oncologist. This lack of disclosure is problematic and is a gap that complementary health practitioners can fill.
While complementary care, per se, is not generally predicted to cause harm, the lack of disclosure and communication between complementary health practitioners and oncologists can contribute to harm. Non-disclosure can result in inappropriate delay of curative conventional therapies. An example of this would be a young man diagnosed with stage IA or IB localised testicular cancer who has been recommended chemotherapy and, instead, seeks complementary treatment. The five-year overall survival after treatment for a man in this scenario is predicted to be 99%. If this man avoids chemotherapy in favour of a complementary approach, he is potentially missing his only opportunity for cure. Once testicular cancer spreads to the regional lymph nodes, five-year survival with chemotherapy drops to 73%.
This situation could likely be avoided with communication between the complementary health practitioner and the oncologist. Another example of potential harm that can result from uncoordinated care is herb/nutrient/drug interactions, which, if present, can interfere with efficacy of conventional treatments or contribute to enhanced toxicities. A classic example of this is Hypericum perforatum, or St John’s wort. While a very effective botanical for depression, if taken concurrently by an individual receiving irinotecan chemotherapy, there is a significant and clinically documented 42% reduction in the levels of the active irinotecan metabolite, SN-38.[3] This would have a dramatic and harmful effect on the efficacy of the irinotecan chemotherapy. Open dialogue between the complementary practitioner and the oncologist increases the odds of a thorough review of potential interactions and the avoidance of deleterious combinations.
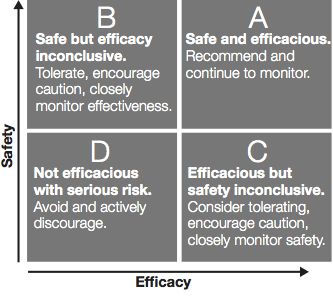
With the intent to create open dialogue present, the question becomes how to best accomplish this. The first condition to establishing fruitful communication is to both practice and communicate certain precepts which are held in common by all practitioners. The first of these might be that both complementary practitioners and oncologists utilise therapeutic strategies for the primary purpose of achieving positive patient outcomes. This unites the work of all practitioners around the good of the patient. Following this, the shared commitment to basing therapeutic strategies on sound scientific evidence is an essential commonality. Evidence-based medicine includes the use of clinical judgement, relevant scientific evidence, and patients’ values and preferences.[4] Thus, communicating one’s judgement particularly about the expected benefit of a given therapy in light of its potential risks conveys reasoned and reliable clinical decision making. Even in the absence of clinical data supporting a complementary intervention,
it is incumbent upon the practitioner to search the database of published science for potential harm or interactions from the intended therapy as well as for underlying mechanisms for the therapy.
Figure 1. Safety vs. efficacy in integrative oncology support
Finally, a third commonality between complementary practitioners and oncologists is the dedication to assuring that patients make fully informed decisions regarding their treatment. This relies upon the practitioners providing full information about all treatment options. While no complementary practitioner can know all relevant information about all treatment options, it is tantamount that the practitioner provides comprehensive information regarding the potential risks and benefits of complementary therapies and refers the patient to an oncologist for a complete review of their conventional treatment options. Additionally, if an established patient of a complementary practitioner refuses conventional oncology care, the complementary practitioner should make appropriate referral for discussion of these implications with an oncologist. This is critical to supporting the patient’s right to be adequately informed about their treatment decisions. If the patient asserts their privilege to not permit sharing of confidential treatment information with other providers, the complementary practitioner should educate the patient about the health and safety risks inherent in poorly coordinated care.
While there is room for a variety of communication styles, there are certain tactical components to make for successful communications with oncologists. Recommendations include the following:
- Establish, at the outset, shared commonalities. Namely:
- identify your intent to provide care in order to enhance positive outcomes and to better the health of your patient.
- state your commitment to using an evidence-based approach to your therapeutic strategy. This might be blatantly and simply stated as, “Utilising published scientific studies, I have evaluated all of my complementary recommendations for their potential benefit and harm.”
- declare your practice of providing informed and full consent. This can be stated along the lines of, “I have provided [patient] with full information about my recommended therapies, including expected benefit and harm.
- Provide a brief overview of the patient’s present health, focusing on their cancer diagnosis, to demonstrate your understanding of their diagnosis and conventional treatment plan.
- Provide a brief description of the intent of your therapies. This may be to improve tolerance to the conventional treatments, to enhance the efficacy of conventional treatment, or to provide specific effects such as immune support, gastrointestinal or cognitive support.
- Include a statement for each biological therapy (i.e. dietary supplement and herbal medicines) that describes any known or predicted interactions with present conventional treatments. Note: this will require searching published literature and/or drug/nutrient/herb interaction databases.
- Provide an outline of the intended duration of each therapy as well as your plan for patient follow-up and assessment.
- Conclude with an invitation to the oncologist for further dialogue.
This type of communication is ideally done at the beginning of the patient’s complementary care. Once this initial dialogue is done, copies of subsequent care plans can be shared with the oncologist, especially if there are any adjustments made.
In an ideal world, these communications will open a mutually respectful dialogue between the oncologist and the complementary healthcare practitioner that is centred around the good of the patient. In the real world, this will not always be the case. There will still be disrespectful communications, uncoordinated care, and triangulated patients. Nonetheless, it is incumbent upon the integrative practitioner to do their best for their patients and seek to establish respectful and cooperative dialogue with their patients’ oncologists. In the event of direct conflict of opinion and/or lack of openness on the part of the oncologist, it is important to align with the decisions of the patient, and if they are committed to conventional care, to be willing to defer to the oncologist. This is for the good of the patient. Ultimately, your communications can strengthen the reliability of your clinical care, bridge the divide between conventional and complementary care, and, most importantly, provide better outcomes for patients.
References
- Vapiwala N, Mick R, Hampshire MK, et al. Patient initiation of complementary and alternative medical therapies (CAM) following cancer diagnosis. Cancer J 2006;12(6):467-474. [Abstract]
- Chrystal K, Allan S, Forgeson G, et al. The use of complementary/alternative medicine by cancer patients in a New Zealand regional cancer treatment centre. N Z Med J 2003;116(1168):U296. [Abstract]
- Mathijssen RH, Verweij J, de Bruijn P, et al. Effects of St. John’s wort on irinotecan metabolism. J Natl Cancer Inst 2002;94(16):1247-1249. [Abstract]
- Sackett DL, Rosenberg WMC, Gray JAM, et al. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71. [Abstract]
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.



