Carla Wrenn, naturopath and educator, provides us with her insights into the important role the integrative practitioner may play in holistically supporting the oncology patient in our latest podcast.
Having worked with our ambassador, Dr. Michelle Woolhouse in a collaborative care model to support cancer patients, Carla describes how she supports the cancer patient to obtain their best overall health, to reduce potential side effects of cancer treatment and to minimise modifiable risk factors to improve their health outcomes. Carla explains the complexity of the challenges faced by the cancer patient and how she supports them through diet, lifestyle and supplementation.
Carla discusses the benefits herbs and supplements may offer for addressing inflammation, hormonal and blood glucose imbalances and stress while expressing caution on their use and discussing the hallmarks of cancer and the all important safety aspects of prescribing natural medicine for the cancer patient.
Covered in this episode
[00:39] Welcoming Carla Wrenn
[03:28] The most common treatment stages cancer patients are in when they first come to a naturopathic clinic
[05:19] Carla’s general oncology support strategy
[06:49] Cautions around patient self-prescription with
[10:03] Working within a support team and using telehealth and online support groups for better patient outcomes
[12:59] What are the hallmarks of cancer?
[14:11] Chemopreventatives
[16:30] Anti-inflammatories
[18:22] Immunomodulators
[20:02] Hormonal modulators
[21:14] Blood sugar regulation
[24:40] Circadian dysregulation
[27:19] Supporting patients through stress
[29:54] The microbiome and cancer
[31:53] Testing the gut microbiome
[34:06] Avoiding treatment fatigue
[36:42] Carla’s advice for practitioners
[38:06] Thanking Carla and final remarks
Key Takeaways
- Natural medicine practitioners can support the oncology patient as part of a collaborative care model through careful dietary and lifestyle measures to support a reduction in physical and emotional stress.
- Holistically, supporting the cancer patient to manage comorbidities and to recover following cancer treatment can be done safely and effectively using natural medicine.
- Caution is required when treating a cancer patient with supplements or herbs while they are undergoing cancer treatment. If there is the potential for risk when prescribing a therapeutic to a cancer patient, it is best to avoid the therapeutic or to engage the patient’s oncology team.
- Lifestyle factors including stress management, exercise and sleep are essential to support the cancer patient.
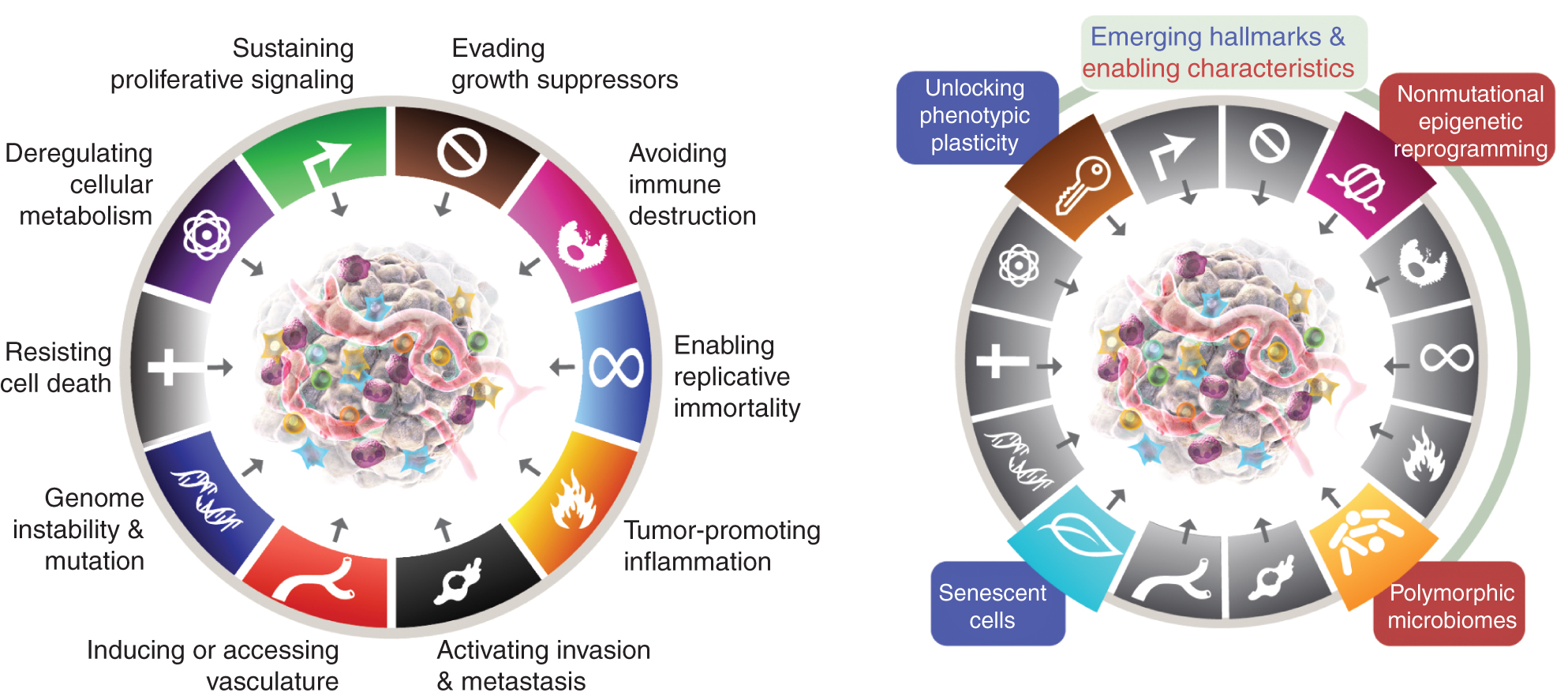
- The hallmarks of cancer support an understanding of cancer management
- Gut microbiome modulation may offer opportunities for gastrointestinal cancer prevention and treatment according to recent research. Functional testing may support this process.
Resources Discussed in This Episode
Additional Resources and Further Reading
Transcript
Michelle: Welcome to FX Medicine, bringing you the latest in evidence-based, integrative, functional, and complementary medicine. I'm Dr. Michelle Woolhouse. FX Medicine acknowledges the traditional custodians of country throughout Australia where we live and work and their connections to land, sea, and community. We pay our respects to the elders past and present and extend this respect to all Aboriginal and Torres Strait Islander people today.
One of the most emotionally complex and, at times, devastating diagnoses is that of the diagnosis of cancer. Cancer is a complex disease that shares the same aetiology of abnormal cell growth. Cancer can arise in almost every cell type and in fact, refers to about 100 different diseases. A recent article published in Tehran oncology in 2019 goes into great detail regarding the deeper meanings of integrative naturopathic principles when it comes to oncology. It encourages practitioners to focus on more than just the disease and to explore with patients other factors, such as overall physical and emotional health, and issues such as intimacy, spirituality and meaning.
Joining us today is Miss Carla Wrenn. She's a naturopath and founder of the Peninsula Herbal Dispensary in Mornington. She's a regular lecturer and educator, and is passionate about supporting people through their oncology journey. She loves sharing the research findings and doing the best for her patients and their families. Welcome to FX Medicine, Carla. Thanks for being with us today.
Carla: Thanks for having me, and thanks for the introduction.
Michelle: So I know you see a lot of women with say, for example, breast cancer, a really common cancer in modern times, and women are particularly focused on holistic well-being. So Carla, let's just start off by what sort of things are women coming to see you for today?
Carla: Yes. They usually come in at one of three stages. They'll come in during the shock, and I would say trauma of the initial diagnosis, looking to really adopt some of those well-being strategies that they've used throughout their life but now feel like they need to be updated and given their current diagnosis.
Then there'll be the patients that will come during the early stages of their treatment because they're starting to experience some side effects. So they might be having hot flashes, or they might be having trouble with insomnia, or maybe they have some kind of other comorbidity that's being flared up by the treatment that they're undergoing for their oncology practitioner through standard oncology.
And then the final group of patients I see, are the ones after their treatment, where they're really looking to pick themselves back up and get back to where they were before their diagnosis.
Michelle: I mean, it's a beautiful way that you kind of shape that, and there's obviously so much that people can do to support that holistic approach to care.
So having worked alongside you with lots of these patients, I can certainly attest to the benefits of having someone like you on the team. Can you share with us your basic general oncology support strategy? And also I guess, how do you kind of see your scope within that holistic oncological team, like me being a GP and we've got sometimes an oncologist, a radiation oncologist, and exercise physiologist, etc?
Carla: Yes. I think that's a really good point. Everyone has such a big part to play. And I certainly see myself as a smaller cog in the wheel. My thoughts are about really how I can support the patient's whole health. So certainly in Australia, and in most other Western countries, patients are getting fantastic care through those oncologists, GPs, radiation oncologists and a lot of the other support team around them. But what is often forgotten, or can be improved is that the patient just feels like their overall health isn't being looked at, or supported in the way that they might need. So like I mentioned, comorbidities.
So those four areas that I really think of is, how can I support my patient to have the best overall health? How can I help them with side effects? How can we adopt some modifiable lifestyle factors like diet, sleep, rest, relaxation that's all published in the research to be shown to improve cancer outcomes? And how can we look after them and their carer to get the best, not only from their oncology treatment with their standard practitioners but also with their whole health and give them a little bit of control back too, so they feel like they're a part of the cog in this big wheel of treatment, as opposed to being an innocent bystander that's just having everything happen to them?
Michelle: Yeah. And I think when I speak to my patients about looking at the whole of their health, they start to feel a lot more empowered.
Can you tell us a little bit about...just break some of those things down in terms of what is your overall aspect of diet, nutrition or insomnia, or lifestyle? Where do you start? Do you have a way or an approach that you start with?
Carla: Yeah. I think we have to remember that, yes, cancer is devastating. And I love that you pointed out that there is around 100 different types of cancer conditions, and that there's really a diverse range of experiences people will have within that. So we consider that in the initial consultation and subsequent consultations, but we also consider those comorbidities or things that might be causing issues.
When we come down to the modifiable lifestyle factors like diet and sleep, I do a really thorough assessment just to see where they're at. We might use some questionnaires to understand the quality of the sleep and how restorative their sleep is. And then we lean into what we've always done as naturopaths or integrative practitioners and support them using some complementary medicines or some education around sleep hygiene, or the appropriate dietary principles for them.
And there's so much evidence on that to how we can incorporate that safely into cancer care. So, if someone is experiencing a breast cancer that's hormonal dependent, we might consider a group of herbs for sleep, but we need to be really mindful that those herbs don't have any oestrogenic action. So the subtle differences are just really around adopting that research, and also ensuring the patient's safety given their current diagnosis.
Michelle: Yeah. Great. So what are the things that you might look out for, for example, using the example that you gave just using herbs for sleep and one of the things that you might want to look out for? Is this something that you see commonly in patients? Because I know also so many people are self-prescribing. I mean, I was at Chemist Warehouse this week and that's an overwhelming experience from a nutritional supplement. Rows, and rows, and rows...
Carla: Definitely.
Michelle: ...of nutritional supplements. And so, lots of people are self-prescribing because some people that have had a diagnosis really are desperate to support themselves. And what are some of your concerns? What are some of the common things that you have seen that you can pick out?
Carla: Yes. So, in two areas, if we go back to that example I gave about the oestrogen-dependent breast cancer and insomnia. If you walk into many different retailers to purchase something for sleep, the majority of those just happen to have oestrogenic herbs in. So we have to be very cautious because our patients, we can't expect them to know this. You and I and many of the audience have studied for years to learn these things. And it just so happens that there are herbs in there that we have to avoid.
So, I do have reservations about self-prescription because there's such easy risk of interactions. Just as a general across-the-board self-prescribing risk, I'd have to say the number one concern I have is the use of curcumin. Don't get me wrong, I absolutely love it and it has a huge amount of research in complementary medicine. But used alongside standard oncology, it can cause some pretty significant interactions. And so, that's probably the one that I see most common. Many people will have it on a dietary level, and that's not so much of a concern. But supplements that are getting higher and higher in dose and bio-availability can be a problem if taken at the same time as some chemotherapies.
Michelle: So in terms of safety concerns, what do you do? Do you avoid it altogether, or is there a timing aspect that needs to be considered?
Carla: Yeah. There's some really great research on this. And it comes down to some calculations to do with the half-life of the medications, and the half-life of the pharmaceuticals, or supplements that the patient is taking. There's a really great guide, it’s called the golden rule that helps us calculate this. But when in doubt, we have to avoid it because there are so many options. I talk to the patients during the initial consultation about the toolbox that they have available to them from complementary medicine perspective. And generally, if it's going to have any risk of interaction, barring a very few exceptions where I might interact and engage the help of the oncology or the pharmacy team within the hospital setting, we would just avoid those. There's always other times to use them, and there's always something else we can use.
So I strongly recommend people getting someone to access and check that safety. The unfortunate thing is the databases that provide all of this information aren't free to access for everyone. So I feel like there's a bit of a challenge there to be able to truly find out all the interaction potentials. But nonetheless, I guess the other warning is sometimes naturals aren't safe, especially when you're trying to combine them with something that's so active, and so important as their standard oncology treatment.
Michelle: I always found it really helpful to team up with a community pharmacist, particularly one that's got an interesting complementary medicine because I found them so helpful at those tricky times as well. And you talk about developing a team. I know you're a big fan of the McGrath Foundation, breast care nurses, and breast support masseurs, and exercise physiologists. Tell us about these supports, and what have you found of benefit working within a more, I guess, specific team for some of your breast cancer patients?
Carla: Yeah. Look, I think the patient has so many different elements to the case. And I think as clinicians, we certainly can't tackle all of those. I think that exercise is a really great...exercise physiologist is a really great example. Again, there's so much research into oncology and the benefits of movement and exercise. But in the scope of the consultation time period that I have and with my qualifications, advising patients on a detailed exercise prescription is certainly not something I can do. And I know that I'm not going to get the best for my patient if I do that.
So engaging someone like an exercise physiologist, or you mentioned, the McGrath Foundation and all of their services, we have a local support group and some really great nurses who are able to provide a different element to what I can provide. And I think the last two years have certainly taught me that patients need this. The systems are intending to be overwhelmed, patients might not be feeling heard as much as they perhaps used to. And so, giving them avenues to get support from other people just gives them more of a cushioning and a feeling of being able to access care from a variety of different clinicians and people who can just support them in different ways.
Michelle: Yeah. I think COVID-19 and all those lock-downs have actually revealed just how much we need support. I know there's a lot of evidence on social support and having support groups or that ability to kind of, I guess, offload a lot of the trauma, or sharing a common human journey...
Carla: Yes. Yeah.
Michelle: ...is so powerful for healing as well.
Carla: One piece of very interesting research that I did see lately is just the amount of information that's suggesting...surprisingly, I was quite surprised, but it'd be interesting to hear what you think is that the research shows that even if patients are to access those services in telehealth or in online support groups, they still get the same benefit as if they were to access a practitioner in a clinical setting, or a support group in a clinical setting. I thought that was quite interesting, given the restrictions that some people will be facing, both in Australia and around the world. So, it's good to know that we can still give that level of care. I just sometimes think more people helping is a better situation at the moment.
Michelle: Yeah. We've been forced into the telehealth role, and the online support groups has certainly been fantastic for some people who haven't been able to get there reduces travel time, increases convenience. And so there's definitely lots of benefits as well.
I've heard you speak about what the evidence has coined, is called the hallmarks of cancer. What do they mean by that? And how do you use that to enrich your oncology support program?
Carla: Yes. So the hallmarks of cancer are really based around some published articles and some extensive research by some of the world's best cancer researchers and clinicians looking at how we can understand cancer. And it's evolved over the last, I'd say 15, maybe even longer years to really encompass the kind of drivers that might be considered in cancer.
Now, this was put together to really help standard oncology choose the type of prescriptions and treatment that might be most appropriate for patients. But we can also look at that from a driver perspective and how our complementary medicines interact and play a part in these drivers. And so the hallmarks or drivers are something we can use as a guide. You could also call them hallmarks of well-being when it comes to complementary medicine. We can ensure that we make and meet all the different targets that we know are going to drive or increase the risk or severity of this cancer affecting the patient's quality of life and length of life.
(source: https://aacrjournals.org/cancerdiscovery/article/12/1/31/675608/Hallmarks-of-Cancer-New-DimensionsHallmarks-of)
Michelle: Yeah. Brilliant. So can we break these down a little bit? Because I know that there's a really beautiful way of shaping them into these five different kind of areas. So, let's start. We've got the chemopreventatives aspects of looking at the role of support in oncology. So, let's break them down because we've got a few. So, what do you mean by chemopreventative? And how do you approach that part of the program?
Carla: Yeah. So chemopreventative is a very, very interesting and it's an area that lots of people will come in natural medicine or will be on Dr. Google at home trying to look at those anti-cancer therapies. And that's really something that we can't use as a term. Chemopreventatives is kind of the most comparable term and really what it's talking about, if we break it down, which is quite different or perhaps what the consumer might be looking for, is that these things can help with some of those hallmarks of cancer. It can help in the research, published research to change some of the ways that cancer behaves in the body.
So chemopreventives are looking at that whole system interaction, and how we can use some of the complementary medicines appropriately - and they're not always appropriate - alongside or at different times of the treatment to really improve some of those key drivers in oncology.
Michelle: So, can you give us an example?
Carla: Yeah. So things like turmeric, which I mentioned before. Things that being one of the most popular prescriptions but we have to be quite cautious of that. Things like green tea, Japanese knot-weed. There's a huge amount, and I guess it's understanding the right time to pull those things out of our toolbox. And I think it lends itself to bring up that comment of, more is not always better.
So with my prescriptions, I'm really trying to drill down what nutrients or herbs, or lifestyle advice, or dietary advice can we use that is the least possible to get these outcomes. So what has lots of different actions? And I think the medicinal mushrooms is one that I like. They're a chemopreventative, and I know we'll talk about them and how they help the immune system shortly. But they also have that chemopreventative action. So, we can use them to get multiple actions. And that's what I try and do so our patients don't end up on a whole plethora of things because that's just another recipe for some safety concerns.
Michelle: Yeah. I'm a big fan of medicinal mushrooms myself. Whenever I look into mushrooms, they blow my mind.
Michelle: So the next thing in this shaping of the hallmark of cancer, we talk about anti-inflammatories. Inflammation is a massive driver. We can see it in a pro-inflammatory, anti-inflammatory form. We know that the body loves to have a really good balance of inflammation as well. But anti-inflammatories, we live in a very pro-inflammatory world. It seems like everything that we do seems to inflame the body. So anti-inflammatory pathways are working to de-inflame the body is a part of this hallmark of cancer. Can you talk to us a little bit more about what you mean by that?
Carla: Yes, definitely. So the tumour promoting inflammation is the key within the hallmarks of cancer, and it's really talking about that micro-environment on a cellular level that the tumour grows in, and the fact that inflammation on a cellular level, but also on a systemic level, is going to be detrimental to the progression of the cancer. I also find that inflammation as we know is so important in so many areas. So I think a lot of the comorbidities that patients are experiencing are also directly related to inflammation. Even if we go to something like depression and mental health, we can see that signs of neuroinflammation.
So getting the inflammation under control in oncology is very similar to getting the inflammation under control in just about every complex or chronic modern disease that has that inflammatory connection. So we think about things like omega threes, again, we think about curcumin, PEA, resveratrol, and just all the dietary and lifestyle changes we can make. Someone staying up late and eating the wrong food and having too much coffee and doing all the things you know that cause inflammation, we need to teach them how to address those things too.
Michelle: Yeah, absolutely. That’s that holistic sort of approach. And exercise is very anti-inflammatory as well. So, but again, not too much and not too little. So, it's all that sense of moderation, which is really inspiring.
So let's get on to immunomodulators. As we know, we're going to talk about medical mushrooms or medicinal mushrooms. So immune modulation is really important because the immune system is where inflammation occurs, it's where the white blood cells do their job, it's where we protect ourselves against viruses, and parasites, and bacteria. So let's talk about immune modulations in that sort of sense of the hallmark of cancer.
Carla: Yeah. So, we're really trying to ensure that the immune system does what it needs to do and is destructive in the appropriate way when these cells are incorrectly formed. And so there's extensive research around the immunomodulators. So from things like melatonin and vitamin C and Astragalus, right down to the medicinal mushrooms, we can see lots of evidence of the way that this can help in many ways in oncology, but particularly around supporting the immune system. And the research on compounds like PSK, which is a real Japanese-based formula are just really exciting. We can adopt that and use mushrooms like Turkey Tail and shiitake, which you mentioned and a whole group of other ones to really encourage the immune system to go back to what it needs to do.
And these are one of the ones that we also have to be careful. Because a lot of the new immunomodulator or immunotherapies that are being used, we have to be cautious with using the mushrooms and things like vitamin C and melatonin. But again, in the right time, provide some really wonderful benefits and great to bring into your diet. You're never going to cause yourself harm by eating mushrooms, even if you're on a treatment. So having those shiitakes or other Reishi, other mushrooms that you enjoy, even just button mushrooms has been shown to improve the immune system. So, get eating the mushrooms.
Michelle: Yeah. I'm a big fan of mushrooms. And then we talk about hormonal modulators. So hormones are not involved in every single cancer, but certainly, some of the most prevalent cancers like breast cancer, prostate cancer, etc. have got a hormonal modulation aspect in their treatment programs. So tell us a little bit about how that works with the hallmarks of cancer.
Carla: Yeah. So like you mentioned, it's not something we assess for everyone. But in someone that's coming with a potentially hormonally dependent or stimulated cancer, we do get some assessment done. So I usually lean into some functional pathology and organise to get some good hormonal assessment done to really understand the pathways, and how that person is metabolising their hormones. Again, we look at things like diet and lifestyle. I'm sure your listeners are really familiar with things like plastics and the effect that they might have on hormones.
So we really try and clean up ways that hormones could be causing some issues within the body and in the cancer itself. And then we use things like calcium D-glucarate, which has some really strong and amazing evidence right down to rosemary, even in the herb form. As a fresh tea, we find that rosemary has an action on stimulating pathways that help with detoxification of hormones.
Michelle: Brilliant. And so the last one is blood sugar regulation. So blood sugar regulation seems to be such a strong driver towards inflammation and insulin resistance and just almost messing up cellular messaging. So tell us about blood sugar regulation as part of this oncology support program.
Carla: Yes. So blood sugar regulation. If we look at the general Western diet and the type of foods that many people might be consuming and very often, they don't understand blood sugar regulation. They might have a genetic tendency to have an issue with insulin resistance or even a family history of type 2 diabetes. And all of these things are complications to the drivers of cancer and certainly activate some of those hallmarks we've been talking about.
And as complementary medicine or functional medicine practitioners, we're really in a great place to be able to educate our patients about this with some subtle dietary changes using the basic bloods to assess what their blood sugar levels might be looking like, and then using appropriately things like Gymnema, talking to them about fibre and the healthy fats and having enough protein all really improve these messages and the problems that can be associated with elevated blood glucose level. That seems to be quite consistent across a lot of the cancers that I'm seeing.
Michelle: Yeah. And I think the other beautiful thing about regulating someone's sugar is how much it impacts somebody's mood. For example, often the oncology journey is filled with anxiety-provoking situations. And so regulating someone's blood sugar actually helps to regulate their mood, regulate their sleep, and just regulate their ability to cope with challenging situations for which they're most likely going to face on a day-to-day, week-to-week basis.
Carla: Yes.
Michelle: So such a fantastic kind of whole person care where you really...you might be focusing on looking at bodily health in lots of ways, but in fact, we're working on mental and emotional well-being as well.
Carla: Definitely. And I think it brings up a good point too. Lots of people will come because of that stress and anxiety and maybe the trauma of the initial diagnosis having significantly changed their diet before I even see them, and especially if they've got a good level of health knowledge. But surprisingly, many of those changes that they make, particularly if they pull out lots of fats or animal proteins mean that their blood sugar regulation is actually worse. And so they're trying to make these really positive changes, but it's leaving them feeling a bit unusual because they're just not having enough carbohydrates or complex carbohydrates, perhaps and balance their blood sugar. And they are getting a bit more lightheaded and there are some of the hypoglycemic symptoms. So trying to show them how to formulate a really balanced diet and still engage in the kind of things that they're trying to do with their dietary strategies, but just make sure it's not leaving them feeling deflated and malnourished as well.
Michelle: Yeah. And I think that's where having a support person there with you, because what I find also about the cancer journey is that often the family members are quite anxious as well. And so, the person experiencing the cancer can sometimes feel like they can't burden their familial support people with additional kind of things that they're doing. And so having that kind of external support person where they can freely discuss really what they want to do can be a really powerful balancing effect for them. So they don't have to burden...well, they're not burdening but they often feel like they're burdening their family members with them.
Carla: Yeah. They're overwhelming them. Yeah.
Michelle: Yeah. That's right. But I wanted to add a couple more. It's not official, but I think there's a couple of other aspects of well-being that are really important to consider, and that being circadian dysregulation. I read an article yesterday actually about our teenagers having the worst sleep in the history of humanity. So quite a large...
Carla: That's alarming, yeah.
Michelle: ...headline in the Conversation yesterday. But so circadian dysregulation is actually associated with hormonal dysregulation and stress hormone dysregulation, and all sorts of inflammatory issues as well. And I think it's a really fabulous thing to talk to people about the importance of deep sleep, the importance of the restorative aspect of sleep, particularly in supporting someone on their oncology journey.
Carla: Yes.
Michelle: Tell us how you approach that, too.
Carla: Yeah. So, I really try and engage them around the quality of their sleep. And I think it's one of the things that you have to dig a little bit deeper with patients. I want to know about their dirty little secrets, like they are on their phone late at night, or...
Michelle: Yes.
Carla: ...I don't know. If they're sleeping in really late, and they're going to bed really late. If you ask a patient how many hours they get, they'll just answer by rote eight hours, but they're not telling you if that's from 2 a.m. to 10 a.m. or something like that. The research shows that that's not ideal. And so really trying to gently educate them in the right direction, if they're having trouble with sleep, give them some really good avenues to support their sleep. And talking to them about, like you mentioned, all the things that are affected by their sleep. Blood sugar regulation is another big one. And if they can make changes to that, it's a much easier and more pleasurable thing to change than perhaps having to give up their favourite foods, or some of the other things that we might ask them to do during this whole thing.
I generally say to them, if they're having really terrible sleep or they've got a terrible pattern, and we talk about doing like a sleep rehab or a sleep reset, and really just focusing for seven to 10 days on all the things they need to do to get an earlier night and a better quality sleep. Whether it'll be starting their wind down time at 5:00 and having their meal earlier, and getting off tech, and having a nice warm bath or having a sleepy tea. Just really establishing new patterns and trying to invest in getting to bed earlier and getting better quality sleep. And they feel like different people. They come having more ability to cope with stress and the situation and quite often, their family members start to do the same as well. So everyone's feeling a bit better for it.
Michelle: And I think it's a lovely expression of self-care as well. It's just such a natural part of our lives. And I really harp on about sleep hygiene and optimising sleep.
And the other thing that I think is really important, we've mentioned it throughout this discussion already is that how stressful the oncology journey often is and how anxiety-provoking it is, but chronic stress is quite a severe issue. The World Health Organization say 80% of all chronic disease has some aspect of chronic stress involved in the aetiology of it. So that being chronic emotional stress, chronic mental stress, spiritual stress, physical stress. The world is a very fast-paced culture and we revere stress, but stress is really important to address in the cancer journey. How do you go about supporting your patients in that regard?
Carla: Yeah. Great question. I feel like they come to me quite often on one of the worst days or periods of their lives and so we go gently. It's like an onion, we try and peel the layers. And so we'll ask the general questions about stress. But I think the more you spend time with the patient and the more the trust is there, sometimes the things and the layers start to come off when we can really get the basis of what's causing the stress and then be able to support that. And like you said, it can be multiple things. But if it's a financial stress or if it's a stress about a loved one, or dealing with the emotions and perhaps the trauma of knowing that your life may not be as long as you expected it to be, they’re big issues.
And so I really try and support them with the nutritionals and herbals that I know may help, but also really engage other support people, whether it be psychologists, counsellors, other services that might then be able to set them on a better path. And we talk about not overnight changes. These are changes that we work on over a period of time, particularly things like financial stress. It's obviously not going to change overnight, but how can they put into place some strategies to start to relieve some of the stress? Can they just organise to talk to someone about it who's a specialist in that area, or confide in someone? And who is their support system? I think social connection and the support system is a huge part of this as well. So how can they lean back on their people or have new people that they can work with on these stresses as we start to unravel what's perhaps been years and years of ongoing stress?
Michelle: Yeah, definitely. Yeah. And that long-term, often when somebody has a significant diagnosis, it can be a fantastic opportunity to make some really significant life changes. But obviously, changing everything overnight is stressful in itself. So going slow is definitely a really lovely approach.
So I wanted to shift our conversation a little bit because I know through our pre-podcast conversations and stuff, we were talking a lot about the incredible new research in regards to the gut biome, and cancer prevention, and even the response to chemotherapy. And also having, I guess, the idea of the gut biome in mind when we deal with cancer in general, but also, in particular, specific gut cancers like bowel cancer or rectal cancer, for example. So tell us the latest research and how you try and incorporate this into your supportive methods.
Carla: Yeah. Excellent question. So, in 2021, a really great study was published that I encourage people to look at called Gut microbiome and its role in colorectal cancer. And that really opened up a whole level of understanding and concise and actionable knowledge around how we can adopt and utilise the microbiome in a number of ways when we're thinking about those gut-specific and gut-specific cancers. So it's a number of different things. We're even looking at how can we assess the microbiome a bit like they might do a faecal occult blood test to predetermine people that might be at risk of colorectal cancer because of the species inhabiting their microbiome.
So really, when my patients come to me with a diagnosis, it's one of the things we must think about for all patients, but particularly for those gut-based oncology cases. And so I'll usually organise to do some form of assessment of their microbiome to discover if they do have any of those species, but also to find out a bit more about what's going on there with digestive enzymes, acids, detoxification profiles, those kinds of things. And getting the microbiome sorted for people with any cancer diagnosis, as you mentioned, helps the absorption or effectiveness of the chemotherapy in new research.
So it's a big area, and I think we're just learning the tip of the iceberg. And I think going forward, they'll probably be so much more to learn. But certainly, something that's important to keep our eye on and then discuss with our patients.
Michelle: Yeah, definitely. So you mentioned testing for the gut biome, and there's a lot of different tests out there. Is there one that you particularly favour?
Carla: It's a tricky question. I think it's like choosing your favourite children. I really do still love the CDSA Level-2 for its basic nature and its actionable information. But then I would also use things like Microba and some of the more advanced testing if I'm trying to get a bit of a bigger overview, particularly if patients have already been through their treatment and we're now trying to provide a microbiome that's preventative or protective long-term. And so really, I choose different tests given the stage that someone’s at. Also financially, what they're able to do. We talked about stress and financial stress, and the last thing you want to do is cause more stress. So it's really about picking what's appropriate for each patient and then using as much of that information to direct the care that we're giving them.
Michelle: And I guess, also, dietary advice and utilising pre- or even probiotics, that kind of thing. Do you ever utilise that without doing testing? Do you find that that is of benefit for some people?
Carla: Yes. 100%. So just even talking to people about fibre and food and why our fibre is so important as a prebiotic, and the kinds of fibres that we can add. I'm a big fan of hummus. It's one of those foods that you can really add to increase the fibre quite simply, most people love it. It's easy to put into snacks or add on veggies. Adding fibre is the start of that prebiotic change. We can obviously use fermented foods, and simple probiotics still have a big place.
So not everyone would be using testing. Certainly, if it wasn't a gut-based cancer, then there was probably a more likelihood that I would be using just some general strategies because there's other things I might be testing or other more important things to address. I think it's just another point to be mindful of too, is that the probiotics are fantastic, and we would consider them generally very safe. But if someone is using a chemotherapy that's having a really significant effect on their white cell count, particularly neutropenia, we have to be cautious because we can actually cause a probiotic infection. So it's one we need to choose a little bit carefully. But very important, you can't go wrong with the food that will help as a prebiotic action.
Michelle: Yeah, definitely. And I think that's empowering for the practitioner, but it's empowering for the patient as well. If there is financial issues or treatment fatigue, and that was the next question I want to talk to you about because this is what I see in my practice is a sort of sense of treatment fatigue. I think often what happens with people with a diagnosis of cancer is their life is going along day-by-day, ordinary, and then bang, this news comes and as you mentioned earlier in the talk, this sense of trauma.
But then there's this enormous change in your life where you're seeing multiple different practitioners sometimes daily, sometimes every week and it's a huge change for people. And what I see is a sort of sense of treatment fatigue. And I know that you would consider this in your patients.
So, how do you support people with that? And I guess from a whole person lifestyle medicine, it's ongoing, ideally. And how long do you try and treat people for? And how do you wrap it up for people? What's your approach there?
Carla: Yeah. So in the first consultation, I really try and highlight the fact that we do have so many options, but the skill is choosing the appropriate option at the appropriate time. And so whether it'll be keeping supplements to the minimum, or just making simple changes, not over overwhelming them. Giving someone a huge dietary handout is something that we're sometimes encouraged to do. But I know just from my experience in clinical practice, they probably never adopt anything out of it if it's too overwhelming. So really just working. If we're working our diet one meal at a time, how can we up-level the breakfast to be more appropriate?
And next time, we might want to talk about how to make some simple changes to get more movement into their day. And so I try and really try and chunk it down and just give them the bits that are most important. Then you have those patients that are really motivated and engaged, and they want to know more. And there's always more we can tell them, but I try and keep it on the simpler side. So then it's something that over time evolves to be a completely new-looking life, and perhaps something that's much healthier, not only for their oncology but also for their general well-being. Family usually makes those changes as well.
And so some patients that I've been working with upwards of 15 years, and looking at how we can improve things. And it's ever-changing, particularly if someone's had an extensive period of treatment like some of my metastatic patients who are on ongoing treatment, the type of things we have to do for their diet or the strategies that we have to continue to change and make so that they can continue on to be as healthy as possible while undergoing those long-term therapies mean that there's always something to learn.
Michelle: Brilliant. I s there any questions that I haven't asked you, or is there something that you haven't said that you really feel is very important for all of our listeners to hear?
Carla: Yeah. I think it's just really important to be mindful of the fact that patients do have so much they can do on this day when they get this terrible diagnosis and the weeks subsequent to that. But there's a lot of support available, and also a lot of research for that support. That's why I got into working in this space and supporting patients undergoing cancer because I was just so inspired by the amount of information that was there to say using particular herbs and nutrients were helpful and effective.
And I think getting the right advice, taking your time not making rash changes, and also really looking at how we can support the patient, but also the carer. And there's a lot of research, one of my colleagues is doing up in Sydney on how we can support the carer, and ensuring that they don't end up having worse health in the long-term, which is what the data shows. And so I think it's just that there are lots of people like you and I, and other clinicians working in this area who are here to help and give the right advice. So walking into some of those retailers, as we mentioned, and grabbing something might seem simple, but I feel like there's a lot of better quality and actionable, and research evidence, and ways to go about it that might as well be more cost-effective in the long run and get better outcomes.
Michelle: Yeah. And Carla, thank you so much for being with us today. I love your idea of the toolbox. I think that's such a beautiful thing because sometimes complementary medicine can be overwhelming and just how much benefit and how much support it can have. So knowing that we've got a toolbox and really supporting patients to understand that we've got choices within lifestyle medicine and within complementary medicine. And there's so much opportunity for patients to improve their health. It's such a vital time in their lives. And the work that you're doing in this space is so important, and just so appreciate your passion, and I know that you're hugely appreciated by your community.
Carla: Thank you very much. Yes. I think it is an exciting time. And it's such a pleasure to work in this space. And yes, I'm very appreciative.
Michelle: So thank you everyone for listening today. And don't forget that you can find all the show notes, transcripts, and other resources that we discussed from today's episode on the FX Medicine website. I'm Dr. Michelle Woolhouse, and thanks for joining us. We'll see you next time.
About Carla Wrenn
Carla Wrenn is an Integrative Naturopath & Nutritionist. Completing a Bachelor of Health Science in 2001 and practicing for 21 years.
As a passionate learner Carla also completed postgraduate studies in Integrative Oncology, Autoimmune Diseases and Functional Medicine within Australia and the USA. Carla’s time is spent consulting in the area of complex and chronic diseases, especially Oncology.
Carla is the owner of Peninsula Herbal Dispensary & Naturopathic Clinic, where Carla works with 12 Naturopaths and a support team, who love providing Acute Care, Consultations and lifestyle retail offerings to their Mornington Peninsula community and beyond.
Carla is a passionate advocate for all we have to offer as Naturopathic and Complementary Medicine Practitioners. She values industry collaboration and has spent the last 6 years training over 1000 Practitioners in her course Vitae Mosaic – Naturopathic Functional Medicine and more recently in the areas of evidence based oncology support and Long COVID.
You can contact Carla and learn more at carlawrenn.com
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.