When aiming to address allergic symptoms, reducing exposure to known allergens is essential. These recommendations can be given to assist in regulating normal immune responses and stabilising mast cells to reduce excessive histamine release.
Nutrition
Quercetin
Quercetin is an anti-inflammatory and antioxidant bioflavonoid. Its mechanisms of action include stabilisation of mast cells, neutrophils and basophils, and inhibition of histamine release (by blocking mast cell degranulation).[2]
Weng Z, Zhang B, Asadi S, et al. Quercetin is more effective than cromolyn in blocking human mast cell cytokine release and inhibits contact dermatitis and photosensitivity in humans. PLoS One 2012;7(3):e33805.1]
Quercetin inhibits the release of pro-inflammatory cytokines from human mast cells, and appears to significantly reduce contact dermatitis, photosensitivity and associated pruritus that are typically resistant to anti-histamines and cromolyn.[[1]
Vitamin C
Vitamin C is known to provide nutritional support for a healthy immune system, plus it acts as a natural antihistamine and is a well researched antioxidant. Lowered vitamin C levels are associated with increased blood histamine levels, while increasing vitamin C status has been shown to decrease histamine levels; being a DAO cofactor, it enhances histamine degradation.
High dose vitamin C has been shown to be a potent immunomodulator, regulating natural killer cells and influencing antibody and cytokine synthesis in some situations.[3]
Vitamin D
Apart from its classical function in bone and calcium metabolism, vitamin D is involved in immune regulation, and its deficiency has been linked to various immune disorders and allergic diseases.[4]
Vitamin D deficiency is common in specific subpopulation groups in Australia,[5] thus it should be considered as an aetiologic factor in the development of certain chronic diseases, including those relating to immune system imbalance.
Vitamin D functions within both the innate and adaptive immune responses, and an insufficiency/deficiency early in life has been identified as one of the risk factors for food allergy.[4] The Vitamin D Council recommends that adults take 5000IU/day and children 1000IU/day to achieve healthy vitamin D levels.[6]
Supporting histamine metabolism
Histamine is an amine produced as part of local immune responses to injury, infection and inflammation. It is a key mediator in the symptoms of allergic reactions and histamine, together with other protective inflammatory mediators, is released in response to allergens. It also occurs, to various degrees, in many foods. Highest amounts are found in processed meats, tomatoes, fermented foods (such as cheese, miso, kombucha, pickles), nuts, strawberries, bananas, tea, coffee and alcohol.
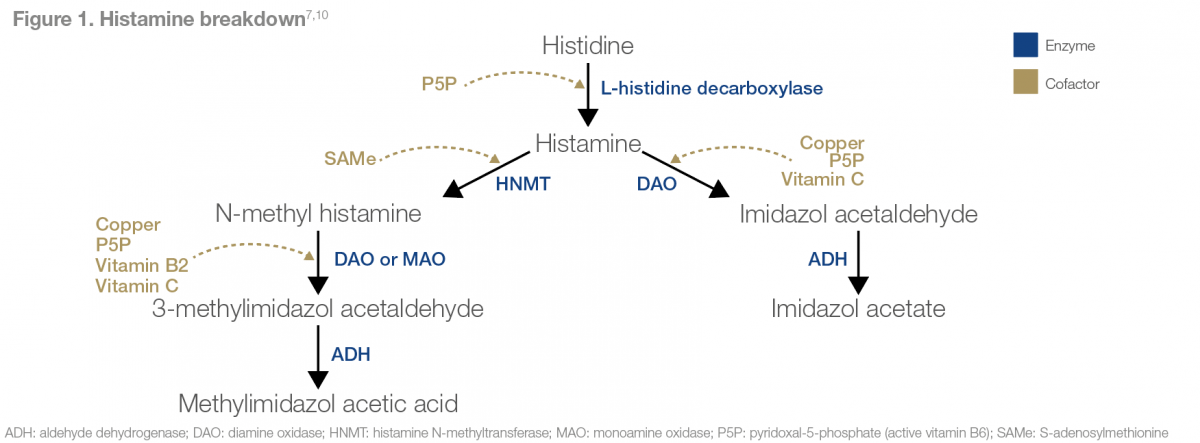
In healthy people, dietary histamine can be rapidly detoxified by amine oxidases (refer to Figure 1), whereas people with low amine oxidase activity are at risk of histamine intolerance. Histamine intolerance results from a disequilibrium of accumulated histamine and the capacity for histamine degradation.
Diamine oxidase (DAO) is the main amine oxidase for the metabolism of ingested histamine. It has been proposed that DAO, when functioning as a secretary protein, may be responsible for scavenging extracellular histamine after mediator release. Conversely, histamine N-methyltransferase (HNMT), the other important enzyme inactivating histamine, is a cytosolic protein that can convert histamine only in the intracellular space of cells.
An impaired histamine degradation, based on reduced DAO and/or HNMT activity and the resulting histamine excess, may cause numerous symptoms mimicking an allergic reaction.[7]
The DAO enzyme is dependent on vitamin B6, copper and vitamin C,[7] while HNMT utilises SAMe as a cofactor.
Stress and cortisol imbalance
It is well known that atopic disease is characterised by an imbalance of the stress-axis response along the hypothalamic-pituitary-adrenal axis (HPA) and the sympathetic axis (SA). Systemically, a shift towards an allergic-type immune profile is promoted under the influence of cortisol and neuropeptides that are released as a result of stress.[7,8]
Furthermore, cortisol has been identified as significantly increased in patients with atopic dermatitis (AD), whilst the severity of AD appears to be correlated with intensity of stress.[9] Consequently, imbalanced stress-responsiveness is likely at the core of exacerbated allergic disease, and stress management should be considered for individuals suffering such conditions.[8]
References
- Weng Z, Zhang B, Asadi S, et al. Quercetin is more effective than cromolyn in blocking human mast cell cytokine release and inhibits contact dermatitis and photosensitivity in humans. PLoS One 2012;7(3):e33805. [Abstract]
- Chirumbolo S, Marzotto M, Conforti A, et al. Bimodal action of the flavonoid quercetin on basophil function: an investigation of the putative biochemical targets. Clin Mol Allergy 2010;8:13.[Abstract]
- Braun L, Cohen M. Herbs and natural supplements: an evidence-based guide, 3rd ed. Sydney: Churchill Livingstone Elsevier, 2010.[Source]
- Suaini NH, Zhang Y, Vuillermin PJ, et al. Immune modulation by vitamin D and its relevance to food allergy. Nutrients 2015;7(8):6088-6108.[Abstract]
- Van der Mei IA, Ponsonby AL, Engelsen O, et al. The high prevalence of vitamin D insufficiency across Australian populations is only partly explained by season and latitude. Environ Health Perspect 2007;115(8):1132-1139.[Abstract]
- How do I get the vitamin D my body needs? Vitamin D Council. Viewed 5 August 2016, [Abstract]
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr 2007;85(5):1185-1196.[Abstract]
- Liezmann C, Klapp B, Peterscor EMJ. Stress, atopy and allergy: A re-evaluation from a psychoneuroimmunologic persepective. Dermatoendocrinol 2011;3(1):37-40.[Abstract]
- Mizawa M, Yamaguchi M, Ueda C, et al. Stress evaluation in adult patients with atopic dermatitis using salivary cortisol. Biomed Res Int 2013;2013:138027.[Full Text]
- Higdon J, Drake V, Delage B, et al. Vitamin B6. Linus Pauling Institute 2014, [Source]
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.



