Do you know a toddler who has out-of-control tantrums, and wonder “Is this just a normal developmental phase or a parenting issue?” Do you know a teenager who is totally ‘normal’ one day, and raging, obsessive, violent, and paranoid with motor and vocal tics the next? Or do you know a primary-schooler who has had worsening separation anxiety and emotional lability, who used to be a great student but is now barely holding on because they can’t focus, and has difficulty processing or remembering what they have learned just the day before?
Then you may know a child who has paediatric acute-onset neuropsychiatric syndrome (PANS) or paediatric autoimmune neuropsychiatric disorders associated with streptococcal disease (PANDAS). And if you don’t currently know a child with PANS or PANDAS – it’s not a matter of if you will, it’s a matter of when.
According to the American Academy of Paediatrics it is estimated at least 1 in 100 US school children has PANS, with that number climbing every day.[1] Many of these children are misdiagnosed, or are just simply missed all together.
A missed diagnosis
According to the PANDAS Parent Survey in April 2014, it took over three years for 35% of children to be appropriately diagnosed with PANS/PANDAS.[2] Another 26% took between one and two years to be diagnosed. That means that over half of all children with PANS will be misdiagnosed and mistreated for over one year. Most children are misdiagnosed as having psychiatric illness, behavioural problems, or parenting concerns. Many go through trials of multiple psychiatric medications and therapies with only minimal benefit. But PANS is so much more than a ‘mental health disorder’. PANS/PANDAS is an immune-modulated, neuroinflammatory encephalitis, and without appropriate antimicrobial, anti-inflammatory, and immune-modulatory treatments, our children with PANS will be facing an uphill battle to get well and heal their brains.
Unfortunately, by the time many children land in our office, they've likely already been misdiagnosed and mismanaged. As functional medicine practitioners, we play a vital role in recognising how children may present with PANS/PANDAS so that they can be appropriately diagnosed and treated as soon as possible. Only then is recovery possible. As with all chronic illnesses, the goal of functional medicine is to treat the root cause. And understanding how to identify the root cause(s) of PANS/PANDAS is the first step in getting our children well and addressing these conditions.
How do you diagnose PANS/PANDAS?
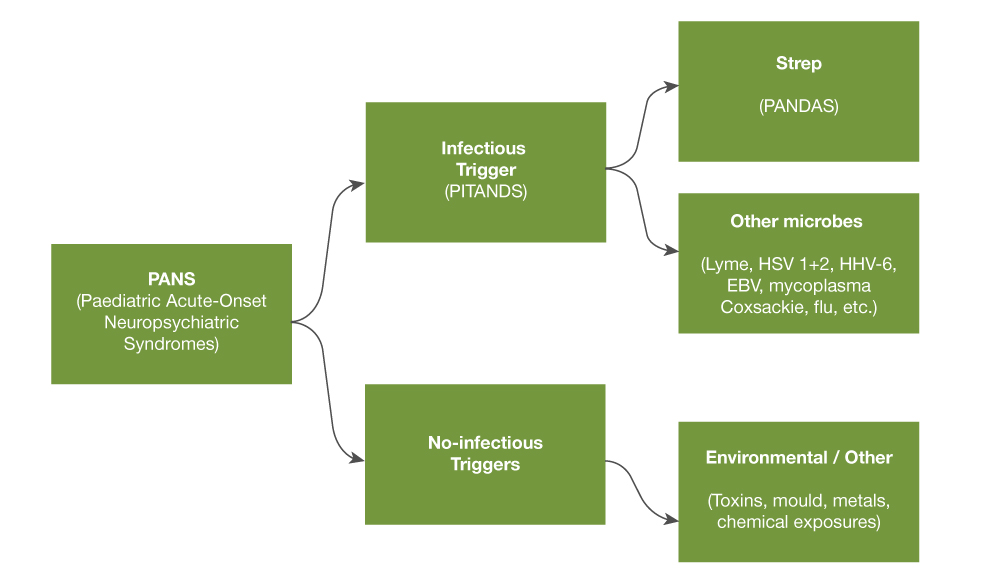
PANS is a neuroinflammatory encephalitis that can have multiple triggers - infectious and non-infectious. Infectious triggers appear to be more common than non-infectious triggers. PANDAS is a subset of infection-triggered PANS caused by streptococcal infection. However, many infections are now known to be possible triggers of PANS - including Mycoplasma pneumonia, influenza, Epstein-Barr virus, Lyme and other tickborne infections, HHV-6, HSV1 and 2, parvovirus B19, coxsackievirus, cytomegalovirus, and candida. Non-infectious triggers include environmental toxins such as mould, heavy metals, and other toxic exposures, as well as metabolic disorders such as diabetes and lupus cerebritis.
Figure 1. PANS and infectious/non-infectious triggers
PANS/PANDAS remain, however, a clinical diagnosis with specific criteria (Table 1).[3]
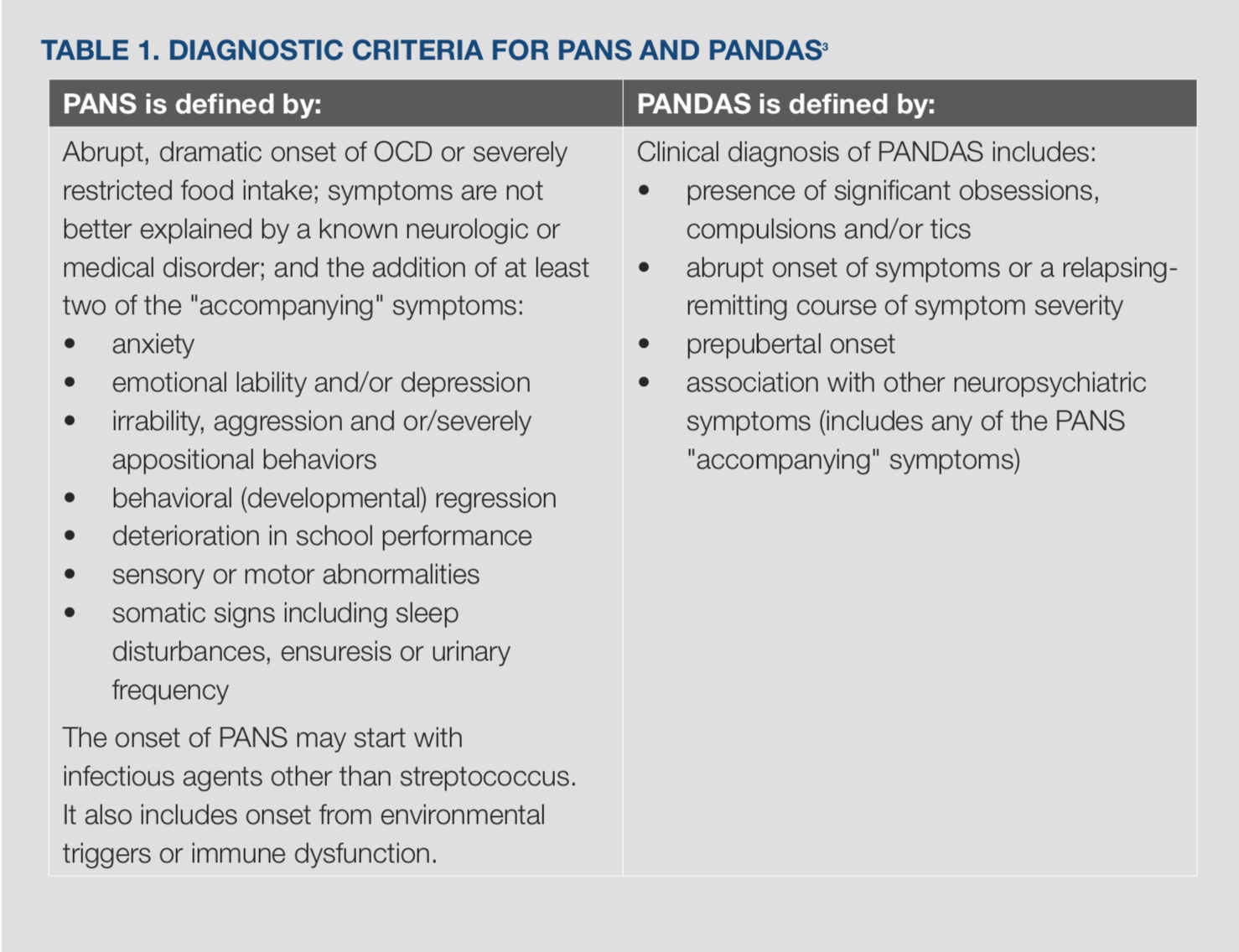
Symptoms of PANS can vary and do not necessarily present as acutely and dramatically as the ‘classic’ cases seen at specialty clinics like the PANS Clinic at the Lucile Packard Children's Hospital at Stanford University. A diagnosis of PANS should be considered in any child who presents with a new onset of the above symptoms, even if neither abrupt nor dramatic.
PANS is a waxing and waning condition with recurrent flares being the norm rather than the exception. Once you have treated a child with PANS, you will never forget the devastating impact that this illness can have on that child and his/her entire family. Proper and early diagnosis is imperative for appropriate treatment, quicker time to remission and improved prognosis.
If you don't look, you won't know, and yet another child will be missed…
Is there a test for PANS?
A landmark consensus statement was released in 2013 for the clinical evaluation of youth with PANS.[4] While PANS remains a clinical diagnosis, the goal of testing is to determine the root causes(s) of this child's autoimmune or immune-modulated neuro-inflammatory encephalitis in order to better target treatment.
Patients with PANDAS have a history of recent or recurrent streptococcal infection that does not necessarily present as pharyngitis. Cultures should be taken of the throat, nasal cavity, perianal/vaginal areas as well any impetiginised skin lesions. Blood tests often reveal persistently elevated antistreptolysin O (ASO) and anti-DNAse B strep antibody levels.
Quantitative IgG and IgM antibody levels should be assessed for other possible infectious triggers of PANS, as indicated by clinical history or suspicion. These may include testing for Mycoplasma pneumonia, influenza virus, Epstein-Barr virus, Lyme and other tick-borne infections, HHV-6, HSV1 and 2, parvovirus B19, coxsackievirus, cytomegalovirus, candida, and others as indicated by the child's history. It should be noted that the presence of very elevated IgG titers (concentration) may represent persistent chronic active infection despite negative IgM titers. While under recognised, this phenomena was noted as early as 1991 with severe chronic active Epstein-Barr virus infection syndrome.[5] Targeted antimicrobial treatment should therefore still be considered for a patient presenting with very elevated IgG titers despite negative IgM titers.
If all antibody levels are negative and no infection is detected, non-infectious triggers must be considered. Appropriate testing should be performed for mycotoxins, heavy metal exposures and other chemical exposures.
Despite the above testing, there will be children with PANS who do not have clearly identifiable triggers. For those children, the Cunningham panel offered through Moleculera Labs in the United States can be a valuable piece of the diagnostic puzzle.[6] The Cunningham panel, developed by immunologist Dr Madeleine Cunningham who has been on the forefront of PANS research, tests for four neuronal autoantibodies (anti-dopamine receptor D1 and D2L, anti-lysoganglioside GM1, and anti-tubulin) as well as activity of the calcium-dependent calmodulin protein kinase II enzyme (CaM kinase II) found to have elevated activity in patients with PANS.
Conventional treatment approaches to PANS
Hot off the presses in July 2017 are treatment guidelines for the clinical management of PANS. ‘Conventional’ treatment for PANS incorporates three arms - psychiatric/behavioural interventions, immunomodulatory therapies, and antimicrobials to treat and prevent infection.[7-9]
From a behavioural and psychiatric standpoint, it is imperative that children work with a psychologist or psychiatrist who understands the changeable nature of PANS. School accommodations should be in place for parental notification of infectious diseases that may trigger a PANS flare, and educational adjustments should be made during these episodes. There will be weeks where children will be completely neurotypical, emotionally regulated and performing beautifully in school, and weeks where these very same children will have debilitating fears, OCD symptoms, tics, memory and cognitive processing issues, severe handwriting decline and emotional lability. Cognitive behavioural therapy and family therapy are important adjuncts to any medical intervention. Psychiatric medications may be necessary in times of crisis for severe OCD, anxiety, depression, ADHD symptoms, sleep disturbance, and other neuropsychiatric symptoms. However, these medications and behavioural interventions are merely bandaids, and often not as effective until the underlying neuroinflammation, infections, immune dysfunction and other root causes are addressed.[7]
As in any inflammatory or autoimmune process, anti-inflammatory and immunomodulatory interventions are often required in order for symptom relief and healing to take place. Increasing evidence supports the pathophysiology of PANS as an immune-mediated neurologic disease involving dysregulation of the adaptive immune response with autoantibody production, and a dysfunctional Th17 immune response. While immunomodulatory treatment for PANS/PANDAS must be tailored to the severity of illness and the child’s individual needs, for children presenting with mild to severe symptoms therapies may include a trial of NSAIDs, a short three to five day oral corticosteroid burst (as would be given for an asthma flare), oral prednisone with prolonged taper or intravenous (IV) methylprednisolone/oral dexamethasone pulse, monthly high-dose IV immunoglobulin (IG) (2g/kg divided over two days), therapeutic plasma exchange or plasmapheresis, and IV rituximab.[8]
Antimicrobial treatment and prophylaxis are critical in the management of PANS and PANDAS. Conventional antibiotic guidelines are more defined for the treatment of acute streptococcal infections associated in patients with PANDAS. The benefit of long-term antibiotic prophylaxis is less clear; however, most children do seem to benefit from prophylactic antimicrobials to reduce the likelihood of a PANDAS flare after repeat strep exposure.[9]
There are fewer guidelines for the management of PANS triggered by non-streptococcal infections such as viral, Lyme and other tick-borne infections, and even fewer still for non-infectious PANS triggered by mould, heavy metals or other toxic exposures.
The role of functional medicine in PANS
As you can see, the conventional treatment of PANS largely involves treating symptoms with cognitive behavioural techniques, psychiatric medications, immunosuppressive therapies, and antibiotics (in the case of PANDAS).
It is here that functional medicine plays an essential role in identifying and treating additional root causes and core clinical imbalances from which many of our children with PANS suffer. These interventions may include supporting the gut microbiome and gut-brain connection with probiotics and glutamine; reducing oxidative stress and inflammation with omega-3 essential fatty acids, antioxidants, curcumin, quercetin, and an anti-inflammatory diet; optimising immune function and the Th17 response with specialised proresolving mediators such as fisetin (a bioactive flavonol) or Scutellaria baicalensis (baical skullcap); optimising nutritional insufficiencies and deficiencies; supporting optimal methylation and detoxification with active vitamins B9 and B12 and liposomal glutathione; and addressing mitochondrial dysfunction with CoQ10, acetyl-L-carnitine and ribose.
It is in functional medicine that the hope lies for many of our children with PANS, to regain balance and optimal function, and find true healing for their bodies and brains. The potential for healing with functional medicine is vast, especially for children with PANS and other chronic illness.
References
- Pupil J. PANS treatments, awareness evolve, but some experts skeptical. AAP News, 2017. [Source]
- Calaprice D, Tona J, Parker-Athill EC, et al. A Survey of Pediatric Acute-Onset Neuropsychiatric Syndrome Characteristics and Course. J Child Adolesc Psychopharmacol 2017; doi: 10.1089/cap.2016.0105.[Abstract]
- What is PANS? PANDAS Network 2016. [Source]
- Chang K, Frankovich J, Cooperstock M, et al. Clinical evaluation of youth with paediatric acute-onset neuropsychiatric syndrome (PANS):recommendations from the 2013 PANS consensus conference. J Child Adoles Psychopharm 2015, 25(1): 3-13. [Abstract]
- Okano M, Shuzo M, Osato T, et al. Severe chronic active Epstein-Barr virus infection syndrome. Clin Microbiol Rev 1991;4(1):129-135. [Abstract]
- Cunningham panel laboratory testing recourses. Moleculara labs, 2015. [Source]
- Thienemann M, Murphy T, Leckman J, et al. Clinical management of pediatric acute-onset neuropsychiatric syndrome: part I–psychiatric and behavioral interventions. J Child Adoles Psychopharm 2017;27(7):1-8.[Abstract]
- Frankovich J, Swedo S, Murphy T, et al. Clinical management of pediatric acute-onset neuropsychiatric syndrome: part II—use of immunomodulatory therapies. J Child Adoles Psychopharm 2017;21(7):1-8. [Full Text]
- Cooperstock MS, SE, Pasternack MS, et al. Clinical management of pediatric acute-onset neuropsychiatric syndrome: part III—treatment and prevention of infections. J Child Adoles Psychopharm 2017;27(7):1-13. [Full Text]
You might be interested in the following podcast:
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.





