Oestrogen receptor-positive (ER+) breast cancer is the most common type of breast cancer. It accounts for over two thirds of all breast cancer cases. But what does ER+ actually mean? And if all women have oestrogen, why doesn't every woman get breast cancer?
Tanya Wells is a naturopath whose expertise is in designing integrative oncology programs that utilise the best evidence-based complementary therapies to support conventional treatments. Today, Tanya takes us through the role of ER+ breast cancer, oestrogen metabolism, relevant genetics and how to support patients to prevent recurrence when in remission.
Covered in this episode
[00:40] Welcoming Tanya Wells
[01:45] Different types of breast cancer
[03:40] Fine needle vs core biopsies
[05:18] The role of oestrogen in ER+ breast cancer
[09:33] Clarifying the term “oestrogen-dominant”
[12:53] Oestrogen metabolism and detoxification
[19:45] Clinically supporting oestrogen clearance
[22:24] Diet in treatment of ER+ breast cancer
[28:21] Intermittent fasting and chemotherapy
[31:16] Additional ways to assist oestrogen metabolism
[33:25] Methylation and genetic connections
[37:27] Testing
[40:37] Integrative care and working in teams
[45:41] DNA repair genes
[48:17] Getting back to basics
[52:30] Fear of recurrence and hyper-vigilant patients
[54:59] Additional red flags
Andrew: This is FX Medicine. I'm Andrew Whitfield-Cook. Joining us on the line today is Tanya Wells, a naturopath who's been practising for over 20 years and she has a special interest and expertise in the research and development of integrative oncology programs, utilising the best evidence-based complementary therapies to work in conjunction with conventional treatments such as surgery, chemotherapy, and radiotherapy. She's visited and worked in integrative oncology hospitals in Europe and Asia and is continually collaborating with other practitioners to ensure her programs and clinic models are continually being developed. Tanya is an experienced lecturer at the tertiary level, including at Southern School of Natural Therapies and Endeavour College as well as the Faculty of Medicine at Monash University. She's written and presented a range of drug-herb-nutrient interactions seminars for medical, pharmacy, and nursing professionals in integrative medicine and she's a contributing author to a range of clinical textbooks. Welcome to FX Medicine, Tanya. How are you?
Tanya: Great. Thanks very much for the introduction, Andrew.
Andrew: Tanya, you've had a long experience in helping people with cancer. Today we're going to be talking about breast cancer and recurrence of ER+ breast cancers, that it's not all about the oestrogen. So I think first, though, we've got to talk about the different types of breast cancer.
Tanya: Yes. I guess we wanted to have a chat about breast cancer because it definitely is the most common type of cancer that you'll see in clinic.
Andrew: Yeah.
The Microbiome and Breast Cancer by Georgia Marrion, Read Article
Tanya: I think the current status is hitting towards one in seven women will have a lifetime incidence of breast cancer. And certainly, as, you know, complementary therapists, we get a lot of patients in looking for that extra help during that process. So the vast majority of those breast cancers are oestrogen-positive or ER+ breast cancers. But I guess the first thing we do need to talk about is the different types.
So when someone's diagnosed with breast cancer or they have a lump, something shows up on a mammogram or an ultrasound, or they feel it, most of the time they'll have a biopsy, which we're looking for one of three receptivity markers. So this includes ER, which is oestrogen, PR, progesterone, and HER2, which is epidermal growth factor receptor. And each of those is determined to be positive or negative, determining whether the cancer cells are receptive to those growth factors or hormones. So the most common types of breast cancer are ERPR+, HER2-negative, which is about 70%, ER/PR-negative, HER2-positive, which is about 20%. Then we’ve got triple negative or basal-like, which means that none of those receptors are positive. And then we’ve got triple-positive, that’s in each. And the treatment and prognosis of each of those types of cancer is very different.
Andrew: Yeah
Tanya: Yeah. So today we thought we’d focus on the ER+ ones though, because they are the ones that are the most common.
Andrew: When we’re talking about biopsying a lump, and you go for fine needle vs core, tell us a little bit about the expectant results of those and really what happens with women.
Tanya: Okay. So the fine needle biopsy is I think, you know, found to be not very effective as a testing tool. A core biopsy is a much bigger sample of tissue that’s taken, but it just means that you are going to get a reliable outcome from that test. The worst thing you want to do is have a fine needle biopsy, or multiple fine needle biopsies and then have to go in an have a core biopsy or something else.
Andrew: As well, yeah.
Tanya: Afterwards though we usually want to go straight to the most appropriate tests.
Andrew: Like I know people would like to shirk on the, or err on the side of less invasive techniques, but I just don’t understand why it’s more than likely that it’s going to progress to have a core biopsy as well, so why would you bother with the fine needle biopsy at all?
Tanya: Well, most of the time you wouldn’t.
Andrew: Yeah.
Tanya: I wouldn’t recommend it.
Andrew: I don’t know, I just don’t understand it.
Tanya: No.
Andrew: When it’s, it’s kind of like you know what’s gonna happen anyway, so why bother with the first one? Cause all you’re really doing is two procedures rather than one.
Tanya: Yes, and you’re more likely to… yeah it just creates more stress, because not only is the most stressful time for patients, the wait between having a test and getting the results, but also you’re going to get a result that’s inconclusive so then you have to go through the whole thing again which is just torturous.
Andrew: Yeah, absolutely. Torturous on many levels. So let's talk about the role of oestrogen in ER+ breast cancer.
Tanya: Yeah. I guess there's a couple of big messages that I'd really like to make clear because, you know, I do, I chat with a lot of other practitioners and most practitioners are very confused about the role of oestrogen. You know, I get questions like, “Well, every woman has oestrogen, so why doesn't everyone get ER+ breast cancer? Is it really causing the cancer? What does it do? How do we work it out?" It's very confusing.
So I guess I wanted to focus on two things today, one to talk about exactly what is the role. Is oestrogen causing damage? And if so, what damage? And then we also want to talk about non-oestrogen areas because the current medical model totally focuses on oestrogen. That is the main long-term preventative support in that you're on an anti-oestrogen of some sort, either something that's going to block its synthesis like an aromatase inhibitor or something that's going to block that binding of oestrogen to the receptors like tamoxifen. So it is not all about the oestrogen, but I guess, firstly, we need to talk about what it does.
So oestrogen, we know of oestrogen as being a growth promotant. It's certainly responsible for our secondary sex characteristics, but it has a role to play in DNA damage. So we have to take a step back then and say, "Okay, well, which people are more likely to have that oestrogenic kind of genotype?" There is such thing as an oestrogen-responsive genotype and some women have that. As a naturopath and complementary therapist, we'd often talk about someone who presents with an oestrogen-dominant kind of clinical picture, and those persons we'd often see who had, you know, early menarche, so their first period was quite young, they seem to have an oestrogen-dominant status, conditions like fibroids at the breast and the uterus, endometriosis, heavy bleeds, PCOS, those kinds of things that tend to look like an oestrogen-dominant picture.
But I guess we do want to look at that person's lifetime exposure to oestrogen, not just endogenous oestrogen but also environmental oestrogens like plastic extracts like BPA, and phthalates, and parabens and other BPAs and so on. So all of those things contribute to your overall oestrogenic status. And the oestrogen, actually, can cause DNA damage, especially if you've had a very long lifetime of exposure to oestrogen. So women who got their period very young, either didn't have any children or have children late.
So we've got a lot of exposure to oestrogen and, of course, we've got breast tissue, which is constantly being stimulated by oestrogen. And one thing we know about in oncology is that the tissues that turn over the most frequently, so those that are replacing themselves really frequently, tend to be the ones where there's more opportunity to make mistakes. There's more opportunity for those cells to make errors when they're replacing themselves. And, of course, in our breast tissue, we've got breast tissue that's developing in the luteal phase every cycle, hoping that your body's going to get pregnant. We've got partial development of that breast tissue and, of course, then it kind of shrinks down again when we get out period, and it grows again, and it's constantly in a state of development and stimulation. So that oestrogen is very important with regards to cause and effect inferences. The way that it actually causes damage is mostly via it being so reactive. Certain types of oestrogen are reactive and they can cause DNA damage.
Andrew: Can I just go back a little bit? You're talking about oestrogen-dominant. I get confused by this because I thought it was kind of like adrenal fatigue. We really had to leave that term behind, that it was oestrogen-driven but not necessarily dominant because, of course, oestrogen is cyclical.
Tanya: That’s right.
Andrew: So is it just a convenience term that we're talking about here or is it actually a dominant type?
Tanya: It is. No, it is a convenience term. I guess I'm going back to, you know, the phrases that I learned when I was studying naturopathy.
Andrew: I do it all the time. Is it true though, we have to leave that term behind that we say oestrogen-dominant, but we really mean oestrogen-driven?
Tanya: Yes, that’s right. I mean, I guess we all say these phrases because they're things that people relate to.
Andrew: Yeah.
Tanya: You know, they can understand what we're talking about on some level, but certainly, there's not a lot of evidence that shows that a person has necessarily an oestrogen-dominant scenario. It is oestrogen-driven and certainly, people have a higher level of active oestrogen…
Andrew: Yeah.
Tanya: …so I guess that's what we need to talk about. What are the factors that contribute to someone having a very high level of these active and reactive oestrogens that are more likely to create problems?
Andrew: And indeed, is it just the hormone? I know that they're hormonally-sensitive receptors, but is it just the oestrogen that causes the cancer given that we've got the inflammatory microenvironment? We've got the two-hit hypothesis, we’ve got the metabolites of the oestrogen. We've got xenoestrogens ubiquitously and continuously in our environment. We've now had researchers testing their friend researchers' poo and... Now, this wasn't in Australia, it was Asia and Europe. But they've tested, not microplastics, but lumps of plastic in their colleagues' poo. I mean, this is not a concern. This is frightening. So we now know, it's unequivocable that we've got constant xenoestrogenic drivers. Correct? Is that right?
Tanya: We do. And certainly, when you test for xenoestrogens, we certainly have ways of testing your metabolites and so on. And that is something that we can test for and we are exposed. There are so many other factors such as, you know, dysregulated metabolism, insulin resistance, inflammation, chronic stress, you know, NF-κB issues, and gene expression, obesity, exposure to radiation, and so on, all of these things contribute to your oncogenic potential in every type of cancer. And there are some that are certainly far more associated with ER+ breast cancers like insulin-resistance. Certainly, that is the number one factor to check…
Andrew: Gotcha.
Tanya: …because we know that insulin resistance can create an inflammatory state which not only promotes growth but can lead to treatment failure. So we have so many factors that are non-oestrogenic that we can focus on as clinicians. And this is where we have a role to play. We have a role to play to add success to someone's treatment program. We have a role to play to create wellness.
Coming back to oestrogen, I think that we really do need to have a chat about, well, exactly getting down to that nitty-gritty, how is oestrogen metabolised? What are the different types, and how are they working in a reactive way? So getting down to that…
Andrew: Yeah.
Tanya: …you know, the real issue in oestrogen is oestrogen metabolism. So when it comes to oestrogen metabolism we have to go back to our very basic knowledge of clinicians and that’s about phase 1 and 2 detox. Liver detox.
Andrew: Yep.
Tanya: So phase 1 detox is converting those raw compounds into intermediate metabolites, and that’s mostly via cytochrome P450 enzymes present in the liver and the breast tissue. And then we’ve got phase 2 pathways. So there are a number of types of oestrogen that can be formed through the metabolism pathways. And we can test for all of these things but certainly the big ones are the 2-OH pathway which is produced by sulfation, 4-OH and 16-OH pathways. And these are the ones, the 4-OH and 16-OH pathways are active forms of oestrogen. They’re far more likely to cause DNA damage because they are reactive. And this is where we actually have a huge role to play in modifying these metabolism pathways to reduce levels of 4-OH and 16-OH and increase 2-OH forms of oestrogen which are anti-oestrogen, in fact they reduce growth and proliferation because they have a very low binding affinity to those receptors. So this is where we can actually use our knowledge of the detoxification process to intervene and change the way that the oestrogen balance in the body occurs.
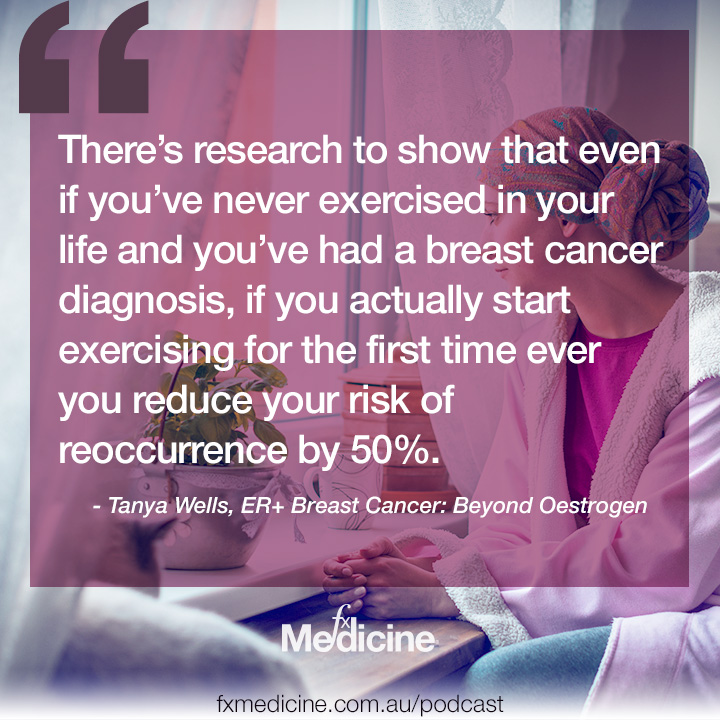
Andrew: And of course one of the best ways we can do this is good old number one treatment from an integrative perspective, or any perspective, and that is exercise.
Tanya: Yes, absolutely. Yeah, I mean look, there’s research to show that even if you’ve never exercised in your life and you’ve had a breast cancer diagnosis, if you actually start exercising for the first time ever you reduce your risk of reoccurrence by 50%.
Andrew: Yeah.
Tanya: That’s better than any treatment combined.
Andrew: Yeah.
Tanya: So absolutely exercise is important. And that’s also important for turning over those fat cells, you know, we store a form of oestrogen, a very active form of oestrogen, estriol, in our fat cells, so we want to turn over those cells to release that oestriol and try to replace it with fat cells that don’t contain as much oestriol. So exercise if very important from a detoxification process but also nutrients important too, like we want to promote the sulfation pathway, methylation pathways, glutathionation and so on, promote production of those inactive forms of oestrogen and we can do that very well nutritionally.
Andrew: Sorry, Tanya, I don’t mean to interject but you’re talking about oestriol or estriol in the fat tissues, not oestrone? Is that right?
Tanya: Yes. Yes that’s right. So both oestriol and oestrone are found in fat. I guess when we think about the main three types of oestrogen that are active in the body, called the parent oestrogens. Oestradiol is of course produced by the developing follicles in the ovaries and that’s our most bioactive form of oestrogen. And then we’ve got oestrone which is found in our fat cells a bit but predominately produced by the adrenals, especially postmenopausally…
Andrew: Yeah.
Tanya: …that’s the main source of oestrogen postmenopausally. And then we’ve got estriol, or E3, which is… it is the major form of oestrogen found in pregnancy, interestingly, and also it is stored in our fat cells. So this is where women who have a high amount of fat, so those women who are obese certainly have a very high level of overall oestrogen but the predominant type is oestriol, followed by oestrone in the fat cells.
Andrew: So can I then ask a question? You know, oestriol was, you know, previously purported to be supposedly protective in pregnancy and that’s why low amounts of breast cancer was seen in pregnancy, but it’s not unfound, there are certainly women that suffer breast cancer during a pregnancy. Would these women be the higher fat content ladies?
Tanya: Not always.
Andrew: Ah.
Tanya: I guess when it comes to recurrence we certainly have evidence that high level of oestriol from adipose tissue is a massive risk factor.
Andrew: Right.
Tanya: I can’t remember the exact statistic but there is a certain percentage of increased risk per five kilograms overnight. I mean that is certainly something that’s significant but oestriol is very important post-menopausally as a risk factor and unfortunately most of the research in breast cancer is in post-menopausal women because of, you know, there’s not much research in women who are, you know, possibly could be pregnant…
Andrew: Yeah.
Tanya: …we don’t have many women participating in research that are pre-menopausal, but certainly all types of oestrogen are important to have a look at and oestriol generally is the least bioactive form of oestrogen that we’ve got there.
Andrew: Right. And so you know we’re talking about oestrogen metabolism, putting it in it’s place about that oestrogen-dominance, but some women do have high oestrogen metabolite issues.
Tanya: Yes.
Andrew: And I know this is not a proven, you know, science, that there still is conjecture about the relevance of oestrogen metabolites but by goodness, I mean, I’ve seen issue after issue after issue when you’ve got high…
Tanya: Definitely, I think there… you know there is so much research and multiple reviews about the role of oestrogen and the types of oestrogen…
Andrew: Yeah.
Tanya: …in cellular proliferation and growth and damage and DNA damage. And certainly, and there’s a bit of disparity between the in vitro research that seems to have a clear result…
Andrew: Yeah. Yeah.
Tanya: …and then the clinical research which is more ambiguous.
Andrew: Yep.
Tanya: And then we’ve got premenopausal and postmenopausal which is, for example 16-OH form of oestrogen does seem to be associated with increased risk if you are premenopausal but postmenopausally, not so much.
Andrew: Ah, okay.
Tanya: So is it that… it depends on where you’re at in your menstrual maturity, but we do want to use these things, you know, clinically as a guide. I’m going to do that oestrogen metabolite test and see exactly what my patient’s current status is. Do they have really high levels of endogenous oestrogen and high levels of these metabolites that we know are active? If we do, if that person does, then we have a role to play in providing support the sulfation, methylation, glutathionylation, and so on to actually promote phase two detox of those active metabolites into more inactive forms.
Andrew: Yeah. When we're talking about that, should we primarily be focusing on, A, exercise, and B, things like fibre in our diet to clear overall oestrogen from being recirculated and then you add other things, you know, just sort of nip things off at the bud to tweak things, or do you go in first with things that have, you know, a really strong effect on the ratios and the levels of the metabolite?
Tanya: Well, I do a bit of everything.
Andrew: Yep.
Tanya: So certainly I would go for the overall microbiome support for high fibre...or not high fibre but good level of fibre diet…
Andrew: Yeah. Yeah.
Tanya: …to make sure that we are getting that oestrogen clearance exercise to turn out those fat cells and promote clearance of oestrogens again. But I guess I do get a bit more specific and individualised with patients. If you're finding that, you know, certain types of oestrogen metabolites are elevated, we might give sulphur compounds to promote sulfation like broccoli sprout extract, sulforaphane, indole-3-carbinol, and so on. Methyl donors of course, and then there's glutathione-rich food that I would mostly use that's supportive in phase two detox. But I guess then we do have to talk about diet as well. I know that there is a huge focus on diets like the keto diet and certainly, we do want a low-carbohydrate diet, especially in people who are morbidly obese.
Andrew: Yeah, of course.
Tanya: But a keto diet is not necessarily appropriate in healthy body weight patients. We certainly want low-carbohydrate but we also need to make sure we're getting plenty of fibre in there for an appropriate microbiome support.
Andrew: So let's take this back to, you know, when a patient presents to your clinic. How much leeway do you have before treatment is going to begin and what sort of dietary measures do you engage in at different times of therapy?
Tanya: Well, I see patients in every part of that spectrum…
Andrew: Yeah.
Tanya: …from, you know, patients saying, "Oh, I've just found out that I've got a BRCA gene and there's no clinical presentation whatsoever,” all the way through to initial diagnosis or precancerous cells, DCIS, and so on…
Andrew: Yep.
Tanya: …through to pre and post-surgery, chemo, radiation, everything, and then follow-up into maintenance and prevention of recurrence. So I get patients coming who have started treatment, who are about to start treatment, or who have finished treatment. It's so variable. But certainly, what I tend to do with ER+ breast cancers is give a overall anti-inflammatory diet. You did touch on this previously about inflammation and we do want an anti-inflammatory diet, which predominantly, the research shows that a pesco-vegetarian diet is most appropriate.
Andrew: Right.
Tanya: And we do focus on that, a low carbohydrate pesco-veg/Mediterranean diet.
Andrew: Okay. So you've got an acceptance there though, like there was some work done by, you know, Valter Longo and others. Indeed, Dominic D'Agostino is doing work... Forgive me, he knows the researchers that are doing other work in keto nutrition during cancer therapy. But, you know, you've got an uphill battle trying to get the acceptance of an oncologist to instigate it.
Tanya: It can be that way. I've found that I don't have a lot of trouble overall…
Andrew: Really?
Tanya: …with communication with oncologists maybe because I've been doing it for a long time…
Andrew: Yeah, yeah. Yeah.
Tanya: …but certainly, the oncologist is quite happy, typically…
Andrew: Yeah.
Tanya: …to interact in a positive way and doesn't usually have much of an opinion about diet. But certainly, keto is very hard for the patient…
Andrew: Sure.
Tanya: …and it's something that's a bit hard to maintain. And although I've definitely read the research about ketogenic diet as being helpful and certainly taking elements from that research is important, but what I've seen clinically is that patients who get too into keto actually put themselves at risk of kidney damage during treatment.
Andrew: Ah, now there's a salient point.
Tanya: Yeah. We have to be quite careful about a ketogenic diet. When you're in ketosis, you do need a huge amount of water intake every day in order to get rid of all those ketones and support kidney function. And certainly, when patients are in chemotherapy, which then gives them further kidney risk. We certainly need to be very careful with implementing that diet during treatment.
Andrew: Yeah.
Tanya: And it's not just that, but also kidney function. I mean, if you look at...
Andrew: It's the biggest red flag you've waived. It's brilliant.
Tanya: Yeah. So it's just the basic knowledge we have about the kidneys. For example, when you look at a kidney function test and you say, “Oh, the glomerular filtration rate should be above 90." Well, actually that's in men.
Andrew: Yeah.
Tanya: A lot of women have a glomerular filtration rate less than 90, naturally, and that's just because most of the research about, you know, what is it appropriate glomerular filtration rate has been conducted in men.
Andrew: Oh my god.
Tanya: So this is where we have to think about that when it comes to the issues around things like ketogenic diet. During treatment, we have to look after our kidneys with women.
Andrew: Absolutely. And, you know, notwithstanding that you're on extremely toxic treatments that have got to be dispelled from the body.
Tanya: That's right.
Andrew: Thank you. Like I really, really thank you. That is a light bulb moment for me. Whereas the Mediterranean style type diet is socially acceptable, culturally acceptable, so much more easy to instigate.
Tanya: There is. And certainly, what you can do is take elements from each of these diets that's appropriate. And it's definitely not a one-size-fits-all program in oncology. And it's not everyone should be keto, or everyone should be paleo, or everyone should be vegan. It's not necessarily the case. Yes, there's certainly evidence about a ketogenic diet being appropriate for certain types of brain tumours or, again, morbidly obese women with ER+ breast cancer may be appropriate or those that have diabetes as well. But when it comes to making it easy for the patient, the patient is in a world of pain emotionally, environmentally, physically, and this is where we need to make sure that as clinicians, we're realistic.
We're looking at this not only from a pathophysiological perspective, but also putting ourselves in that patient's shoes and going, "What could I cope with if I was in this space? If I was having to cook for myself, do everything for myself and I didn't have that support team doing it for me? And, even if I do have a support team, you know, what can I expect from them to be able to make me and support me with a low-carbohydrate, Mediterranean pesco-vegetarian diet if appropriate?" And if you want to take elements from other research, this is where we might do a little bit of intermittent fasting. Fasting pre- and post-chemotherapy may be helpful. Exercise on the day of chemotherapy is certainly been proven to be helpful. You know, we take elements from the rest of that research to try to tailor each person’s plan, individualise it to make sure that we’re maximising the successful outcomes and then we’re supporting them in every other way, including supporting their liver and kidney function.
Andrew: Can you just reiterate the fasting, the intermittent fasting around the chemotherapy episode?
Tanya: There’s a lot of research emerging about intermittent fasting…
Andrew: Yeah.
Tanya: …and most of it is breast cancer. There’s multiple types of intermittent fasting. So there’s extended overnight fasting which can be helpful, certainly that’ been shown to improve insulin-like growth factor levels, it does reduce inflammatory chemical levels, inflammatory mediator levels, and so I do recommend an extended overnight fast on an every day basis. So 13 to 15 hour extended overnight fast, especially in women who are overweight or obese. But around chemotherapy it’s more about having a 24 hour fast before or after chemo, especially before, that it does induce a mildly, I don’t want to say ketogenic, but it is kind of a mildly ketogenic state, where you actually do have a fast just prior to having chemotherapy and that puts those cancer cells in a glucose depleted state.
Andrew: Yep.
Tanya: If women are morbidly obese and they have ER+ breast cancer, it is the case that those cancer cells do use up more glucose than those surrounding cells. But having that intermittent fast prior to chemotherapy puts those cells in that sort of relative glucose deficiency, you have the chemotherapy and then straight away have a snack…
Andrew: Yep.
Tanya: …and that means that the cancer cells are going, "Ah, sugar. I'm going to have, you know, a carbohydrate snack that's going to increase absorption of the glucose and the chemotherapy into those cells."
Andrew: Yeah. So, sorry, I just want to get this clear in my mind because I battle with this. So what you're saying is just fasting more than prior and then, just prior, you have a little snack?
Tanya: Just during treatment, you have a snack.
Andrew: During treatment, you have a snack.
Tanya: Yeah.
Andrew: Gotcha.
Tanya: A healthy, you know, complex carbohydrate snack, but certainly, you don't want to have, you know, a Scotch Finger biscuit or something. But certainly, a healthy complex carbohydrate snack is going to, you know, improve theoretically and certainly according to some in vitro and in vivo research that shows that it does support transport of the treatment into the cancer cell. So it is trying to tailor the chemistry of the body in that exact moment to improve delivery of the chemotherapy to the target cells. It's very difficult.
Andrew: Okay. And, you know, obviously you've got challenges there. We've spoken about the oestrogen metabolites, briefly. Let's go a little bit further into that. What exactly do you use and why?
Tanya: Well, when it comes down to actual treatment, you know, apart from our anti-inflammatory diet, exercise, we're really wanting to support that person's stress response, immune system, and so on. I guess when it comes down to the nitty-gritty of oestrogen metabolism, we do need to make sure that we've got appropriate support for each of those phase two pathways. So sulfation pathway, I mean, the broccoli sprout extract definitely has shown to be the most powerful extract. And so, you can actually just make your own broccoli sprouts or you can get a broccoli sprout extract like sulforaphane, which has been researched as an independent sulphur compound…
Andrew: Yep.
Tanya: …to not only support sulfation but also be anticancer. It certainly switches on DNA repair genes and it has multiple other roles in an anticancer pathway. But there's others too like indole-3-carbinol, diindolylmethane, and calcium-d-glucarate that are all involved in sulfation. And I do tend to give all of those as a package to support that sulfation pathway rather than just broccoli's sprout extract or sulforaphane. I do find that when I'm monitoring patients, so I do tend to do some oestrogen metabolite testing as a baseline and then every three or four months to check-in and make sure that we are tailoring those doses required for that individual in real-time, making sure that we are keeping up to date with how the oestrogen metabolite balance is going. And I do tend to give all of those sulphur compounds as well as methyl donors to support methylation and, of course, glutathione either as a supplement or as glutathione-rich foods.
Actually, I did want to make a point there about methylation in that this is where you might want to do the MTHFR test.
Andrew: Yeah?
Tanya: Certainly, there was a review in 2017 that showed that the MTHFR C677T mutation is far more common in ER+ breast cancer patient population.
Andrew: Ah, okay.
Tanay: So it is something that, you know, if you've got someone who does have that MTHFR mutation, it may contribute to poor methylation, which then has an effect on oestrogen metabolites.
Andrew: When we're looking at methylation, do we want to be doubly sure that we're handling everything that happens with quieting the genes, if you like? So when you're talking about the sulforaphane, the broccoli sprout extract that we're making sure that we are doing the best that we can for that patient to actually get rid of the drivers of those cancers, not just "looking at methylation.”
Tanya: Yes.
Andrew: Is that something you're like just really, you know, on the ball about?
Tanya: Absolutely. But when it comes to DNA, and DNA repair, and DNA mutations, gene mutations that may actually contribute to ER+ breast cancer recurrence, there is a huge body of research about that and certainly, we can certainly delve deeper into that with regards to...there's a few key, you know, cancer susceptibility genes that we do need to be aware of.
Andrew: Yeah.
Tanya: It’s not all about the MTHFR, it's not all about sulfation. We do need to step back and look at the bigger picture and say, "Okay, these are all of the things that we know are relevant in this situation and try to prioritise accordingly." And certainly, we may have information already that that person has presented about their genetic status and whether they have any gene mutations or SNPs or whatever they might be testing for. And then we actually can intervene in those processes as well. It's a pretty common scenario that a patient comes in with genetic testing that's already been done.
Andrew: Ah, okay. Yep.
Tanya: And…
Andrew: I got to say, I wonder if the day is coming where we'll just carry it around like we always carry around our driver's license. It's something that we have, you know, whether we want to use it or not, well, that's our own choice. But I guess the problem is people who don't know what they're carrying around or what they're doing, you know, there's always that concern.
Tanya: And even if you do, it's not necessarily a done deal. You know, I know a lot of patients who say, "Oh, well I've got this gene, so therefore, you know, I'm going to get this type of cancer." That's not true.
Andrew: No. That’s right.
Tanya: We actually have ways of intervening in the expression of that gene and there are ways of switching on DNA repair genes. But, you know, downregulate the expression of all sorts of oncogenic gene mutations. We have a lot of impact in this area and we know a lot about it. For example, BRCA gene, you know, the BRCA gene is a tumour suppressor gene involved in DNA repair, and this does contribute to incidence of breast cancer, but it doesn't seem to relate too much to reoccurrence. But certainly, women who have a BCRA gene, I think there's something like 50% to 70% lifetime risk of breast cancer versus 12% with no BRCA. But, and it also contributes to ovarian cancer incidents. But, you know, we used to think that some substances like genistein and indole-3-carbinol only targets the oestrogen receptors but…
Andrew: Yeah.
Tanya: …now we know that those natural medicines actually downregulate the expression of the BRCA1 and 2 genes themselves, you know, they’re the molecular targets, not necessarily the oestrogen receptor. So we have a growing body of research that shows an intervention is possible when it comes to existing gene mutations.
Andrew: We have so much of a rabbit hole to go down there, Tanya, but let’s pull it back a bit. Let’s go down a little bit further into testing. What testing do you do, and why?
Tanya: Well it depends on the patient, certainly it depends on how they’re presenting and their other known disease states, but I guess general things I would test for, I would definitely do a dried urine oestrogen metabolite test.
Andrew: Yep.
Tanya: You know, there’s been, I was actually just reading about this the other day, about whether that test is actually valid. It does definitely seem to be more valid than just a standard blood test, it certainly is telling us a lot more about the way that the body is working, and I do tend to use that urine metabolite test more than serum testing. I would definitely do MTHFR testing. I also look for other nutrients that are relevant when it comes to phase one and two detox, like selenium. Vitamin D levels. I often do a cytokine profile because I want to see what some pro carcinogenic interleukins like IL-6, so the insulin-like growth factor levels are. And sometimes I’ll do CTC testing, circulating tumour cell testing. It is very expensive and I don’t always think that it’s relevant…
Andrew: Yeah.
Tanya: …to do that. I like to see what’s happening in the chemistry of that person’s body at the time and that’s why the oestrogen metabolite test really is important because it's looking at not only the different forms of oestrogen that had been broken down, also looks at your level of BPA, cortisol, and cortisone levels, melatonin and other things that are relevant from an anticancer perspective.
Andrew: And what about frequency of testing? I mean, obviously, you know, for instance, if you're going to be looking at something that's going to influence oestrogen metabolites, you want a baseline and then you want to see if you've done good work.
Tanya: That's right. All of this, of course, is dependent upon whether that person's taking an aromatase inhibitor. When you’re, if you're on an aromatase inhibitor, that pretty much puts your oestrogen levels at zero because it's reducing the conversion of testosterone to oestrogen. So, you know, that's going to skew the results. But if you've got someone who is not on an aromatase inhibitor, you do want to take that oestrogen metabolite tests as a baseline, then you are implementing treatment. So you're obviously, stimulating sulfation or methylation or glutathionylation. And then I would tend to test about every three or four months. Three months at the beginning just to really make sure that we are individualising the dosage for that patient and making sure that we're changing it kind of in real-time.
Andrew: Yeah.
Tanya: We really want to see the impact of that treatment. And you could do it every two months if you really wanted to, but I'd say every three months just so that we can check in on that particular part of the treatment and support plan and make sure that we're having an effect. You know, we want to make sure we're monitoring that.
Andrew: We've spoken about what do you do if the levels are high, what about really high? Like, what about dangerous?
Tanya: You know, that's where you have to look at integrated care in a way that is appropriate for the patient. And we do often give much higher dosages of support from a complementary medicine perspective. And that's definitely where an argument for an anticancer anti-oestrogen therapy from a medical perspective is very reasonable. You know, you want to make sure that they are intervening on multiple levels, not just with natural medicine.
Andrew: Yeah. And then obviously, you've got the issue of recurrence and you've got the issue of, you know, more than one cycle of therapy and how people fare with subsequent cycles. Particularly when you've got, let's say, somebody who's obese, they've got a real risk of recurrence because of their body weight, their type of cancer. So you've got a whole pot of negative influences there, motivation, you know, how they're fairing during their cycles of therapy. How do you address all of these things with a positive outcome and hopefully reaching a positive outcome?
Tanya: Well, I think one of the things to be is realistic as a practitioner.
Andrew: Yep.
Tanya: I’m very lucky in my clinic. I have a fantastic team of practitioners, including an exercise physiologist, acupuncturist, counsellors, psychologists who, you know, are there as a holistic support team. You know, we're a team of practitioners who are supporting patients irrespective of where they are and that treatment spectrum and their experience of oncology, whether they're a new patient or certainly in that prevention of recurrence space. And having someone, it's all very well us as complementary therapists or naturopath saying, "I need to exercise and this is what we need to do."
Andrew: You do it when you feel a hangover.
Tanya: Well, we've got to get a bit more specific. So, you know, supporting patients to lose weight slowly. We don't really want to lose weight too quickly. That actually liberates oestrogen from the cancer cells. So we do want to make sure it's a steady, slow weight loss, no more than about a kilo a week.
Andrew: Yep. Great.
Tanya: And although, you know, we do also hear that as an excuse. You know, I definitely have heard that with patients saying, "Oh, my doctor says I can't lose weight quickly." We're not asking you to lose five kilos a week.
Andrew: Yep.
Tanya: We’re saying a half to one kilo a week, which is reasonable. And certainly, when you're morbidly obese and, you know, if you're projecting ahead, that's two years of, you know, restrictive diet and exercise that you're looking forward to, you definitely need plenty of, you know, emotional support to help you through that and realistic chats with a practitioner who's going to, you know, refer to a team of support people to help that person throughout that process. It's not easy.
Andrew: Yeah. Look, I've got to say, like that one kilo a week, when you're thinking about a long-term issue, they haven't gotten overweight overnight.
Tanya: No.
Andrew: So we're talking about something that's a learned or a habitual thing.
Tanya: But it's actually, it's not just about losing weight, of course. We want to make sure that we're supporting the chemistry of the body. For example, you know, I have a little rule and that is that, you know, you must have your cardio exercise and your weight-bearing exercise or stretch exercise to a one to one ratio, because people think that they have to just do cardio to lose weight. In fact, that can be counterproductive. Doing an excessive amount of cardio increases your cortisol levels over time, which then actually can promote an inflammatory process. So we do want to look at the big picture again and say, "Okay, well, we need to increase your muscle mass." We do a little bit of weight-bearing exercise combined with a fairly low-carbohydrate, you know, Mediterranean diet and just start to have a look at our portion size. I don't recommend calorie counting or anything like that, it’s not helpful. And so, we want to just sort of do it by bit, by bit, by bit to change those habits and promote wellbeing and all of that requires, you know, a team of people, especially exercise physiologists. Having someone on hand who can help with that on a very practical level, it's a real win from a clinical perspective.
Andrew: I've got to say from the work, I think it was Edith Cowan University in Western Australia, have an exercise physiologist come to the fore lately.
Tanya: They certainly have. And, of course, you can, you know, also have some subsidised consultations with them and they certainly know their stuff.
Andrew: Certainly know their stuff, but good effects in cancer therapy and in cancer outcomes, brilliant, brilliant work that they've done there.
Tanya: Absolutely. And cardiovascular disease and often they go hand in hand.
Andrew: What can you tell us about DNA repair genes, Tanya?
Tanya: Okay. So certainly, DNA repair genes is absolutely the talk of the moment and everybody who comes in as a patient, I mean, I've got plenty of patients who come in and they have already spent the last two months pretty much on Dr. Google trying to learn everything they can about DNA.
Andrew: Right.
Tanya: I guess when it comes to a clinical perspective, we have to again step back and say, "Right, what do we definitely know about cause and effect inferences when it comes to DNA repair genes and what effect they can have?"
Most of the research is unfortunately in vitro. So what we have to do is just draw from that what we think is relevant. So we did briefly discuss before about the BRCA1 and 2 genes and how, you know, that is something that the research has shown that the genes themselves can actually be a molecular target to treatment rather than...you know, we've definitely got receptor-focused research up until this point.
But then we've got other things like the TP53 or p53 gene, you know, this is a tumour-suppressor gene that has been shown to be mutated in over 50% of cancers. Now, there's really not a medical intervention, but certainly, there's a lot of research about it. We know from in vitro research that say, for example, curcumin can convert a mutated p53 into a functional wild-type p53, which begs the question, does curcumin actually only work in patients that have a mutated p53 gene rather than the functional wild-type, you know, there's questions there. But we've got other natural medicines that have been found to have a switch on repair of the p53 gene. Resveratrol, curcumin, as I said, green tea extract, genistein. And these can be quite important preventative strategies…
Andrew: Yeah.
Tanya: …given that we know that, you know, DNA damage occurs over a lifetime. So, in prevention of recurrence, we definitely want to be focusing on some of these other DNA repair genes and just switching them on as a matter, of course, in order to just add to the reduced likelihood of getting a recurrence in the future.
Andrew: Sure. This is really interesting stuff, isn't it? I mean, you're talking about the repair of, you know, something that's been damaged with the, I mean, two-hit hypothesis, for instance. Wow.
Tanya: Oh, it's absolutely fascinating. But, again, you can kind of get stuck in a rabbit hole. And if it sucks you in as a clinician, you know, we really want to know about that kind of thing, but we also want to get ourselves out of that hole and go, "Okay, how can we actually...let's get back to those cause and effect inferences that are modifiable processes. Let's see how we can intervene in this person's body's chemistry to reduce risk of recurrence in the future and kind of bring it back to those practical levels.”
Andrew: And when you're talking about practical levels, you know, like you think about curcumin, you think about where the research came from. It came from curries.
Tanya: Yeah.
Andrew: And how much of this stuff can we incorporate into a patient's diet and lifestyle and show them how to eat a little bit differently and then over time, maybe, if they needed to, a lot differently, you know, having a far healthier diet that's going to actually be repairing their DNA, their genes. I mean, that's a powerful thing.
Tanya: It's very powerful and certainly it does go back to naturopathy 101…
Andrew: Yeah.
Tanya: …where we're talking about, you know, food medicine, but it comes, it is something that, you know, often when patients are in an active cancer process, they may need supplementation and the intense supplementation, like high dose supplementation of key nutrients in an evidence-based way. But then I guess when it comes to general prevention of recurrence and really just stepping back again and saying, "Okay, well, what are we going to do as practitioners? What are the big take-home messages here?"
Certainly, we want to assess those risk factors and choose those interventions appropriately. And that requires quite a lot of background research. You know, working in oncology is not easy. We not only have to know about our own meds and what that can do but also how it's going to interact with conventional medicine, which is another complex issue.
Andrew: Another complex issue.
Tanya: But I guess when we come back and we say, "Okay, what are we going to do here?"
Andrew: Yep.
Tanya: There are some easy things that as a clinician we can support patients. We can look at bodyweight and certainly that's often the elephant in the room from a patient's perspective, and we do need to have frank conversations about it and do some motivational interviewing techniques just to help patients prioritise that. But there's key things, exercise, definitely, especially weight-bearing exercise, you know, a little bit of extended overnight fasting or key fasting, reducing alcohol, of course, because alcohol is the number one environmental toxin that causes mutations of DNA.
We do want to look at the stress response. Stress response, of course, leads to higher inflammation, which can then lead to alteration of the microbiome and breast cancer promotion. So we do want to focus on, you know, the insulin-like growth factor in insulin signalling. And, you know, there's so many other things, general diet support of making sure that you don't have too much exposure to light at night. You know, shift workers need that extra support. So there's the general things that actually make a huge difference and just implementing a good healthy whole food, low meat, low dairy, low carbohydrate, but high nutrient-dense, varied diet is one of the first things that we can do, and that's pretty easy.
Andrew: I remember Liz giving me a very salient lesson about eat a rainbow every day but not including Textas.
Tanya: That's right. Every day, sometimes it's a bit hard. I get people to look at, okay, let's have a rainbow, you know, week, make sure that we've definitely got every colour. And that's the thing. You know, sometimes we just need to give the right easy recipes, give ideas of what we eat…
Andrew: Yeah.
Tanya: …you know, to help patients, you know, come up with new ideas. We tend to eat very same-sy.
Andrew: Yeah.
Tanya: Nice to have some new ideas.
Andrew: Yes. So about preventing recurrence and, you know, one of the elephant in the room is the ongoing hyper-vigilance of patients. How do you address that?
Tanya: That's a really tough one. And that is something that's very difficult to manage. Certainly, the fear of recurrence and that tendency to be hyper-vigilant is completely normal, so what we're wanting to do is just rationalise it, work out how we can live with that reality. We definitely have psychologists here who are very experienced in supporting patients to manage fear of recurrence. And I guess this is a thing when you've got a practitioner who is supporting you in prevention of recurrence or known prevention of recurrence strategies, obviously there's never a guarantee about that but certainly, there are known prevention of recurrence strategies that when you are implementing them as a patient, it gives you a huge level of confidence in your future. So you're not just flailing at the end of your process, medical procedures and just off on your own. You are actually following a plan…
Andrew: Yeah.
Tanya: …and that plan can give you a confidence in and reduce that fear of occurrence. It is something that's really important because, you know, when a patient's in the process of having treatment, they are just putting one step in front of the other, getting through the day…
Andrew: Yeah.
Tanya: …getting through the next treatment and there's no time for processing. It's at the end when, you know, the doctors are like, "Oh, well, you don't need to come back for another six months. Off you, go get back to your life." You know, that person is sitting there going, "What? What do you mean get back to my life? My life is never going to be the same."
Andrew: It's changed. Yeah. That's right.
Tanya: And patients are, you know, in that perfect space to actually have almost like a post-traumatic stress disorder present itself.
Andrew: Absolutely.
Tanya: And that's when that person really needs psychology support. So that's where it's very important to have key practitioners who are experienced in psycho-oncology support to be able to help that person in that moment. And then for us, you know, our role is to help that person have a plan. Have a plan of enhancing wellness, reducing risk factors and that actually gives you a huge level of confidence in the future.
Andrew: We’ve learnt so much from your expertise here today, Tanya, I’ve got to say. And you’ve given me a couple of bricks to the head which have woken me up about a red flag, and that was renal disease when you’re looking at what diet to initiate and so we’ve learnt about that. What other red flags do we need to be mindful of, just quickly?
Tanya: I guess the other red flags are just… I mean the biggest red flags of course is looking at drug-herb interactions and drug-nutrient interactions…
Andrew: Yep.
Tanya: …and any other preexisting conditions but from a preventative recurrence perspective, you know, we’ve got young women, you know, if we’re talking about ER+ breast cancer specifically, you know, most of the patients I’m seeing with that presentation are between the ages of 40, or 30, and 60. Cardiovascular disease is not necessarily the number one issue there, but certainly drug-herb interactions is definitely one of the biggest red flags that we'd be looking out for to make sure that anything that we're going to promote isn't going to interfere with any other treatments.
Andrew: Sure. Tanya, I cannot thank you enough from a personal level but I just, your expertise shines. Tanya Wells, thank you so much for taking through just a glimmer of your expertise today on FX Medicine. I personally truly thank you. I'm so honoured to meet you and have you on the show.
Tanya: Thanks very much, Andrew, it’s my pleasure.
Andrew: This is FX Medicine. I'm Andrew Whitfield-Cook.

DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.