Chronic stress is a major problem, with stress-related presenteeism and absenteeism costing Australian employers $10.11 billion a year.[1] Adding to this burden are the effects of illness, particularly in the winter and autumn months. A 2016 Absence Management Report collated by the Australian Human Resources Institute (AHRI), stated the most common reasons for absenteeism are minor illness, then family/carer responsibilities and finally recurring medical conditions.[2]
These figures provide valuable insight into the level of stress and illness-related stress faced by many Australians every day. The problem is that in the winter months more emphasis is placed on immune stimulation and modulation, to overcome and prevent common respiratory and other immune based conditions, whilst support for the adrenal glands may not even be considered.
Adrenal function and immunity are intricately linked
In 1956, Hans Seyle first linked stress with increased glucocorticoid secretion, adrenal hypertrophy and thymic involution in animals. He showed that stress affected both adrenal and immune function.
In the winter months, adrenal and immune dysfunction may be even more prevalent as all stressors, including seasonal stressors, cause imbalances in energy homeostasis. This is more evident when living in extreme temperatures or with inadequate heating.
However, seasonal stressors affect all individuals to some extent depending on the situation, the health of the individual and differences in perceptions and coping strategies. When temperatures are low, glucocorticoids are released and energy is mobilised to restore homeostasis. If the individual is not able to restore homeostasis, or the stress is sufficiently chronic or severe, immune function may be impaired because energy is directed elsewhere and the adrenal glands are overworked.
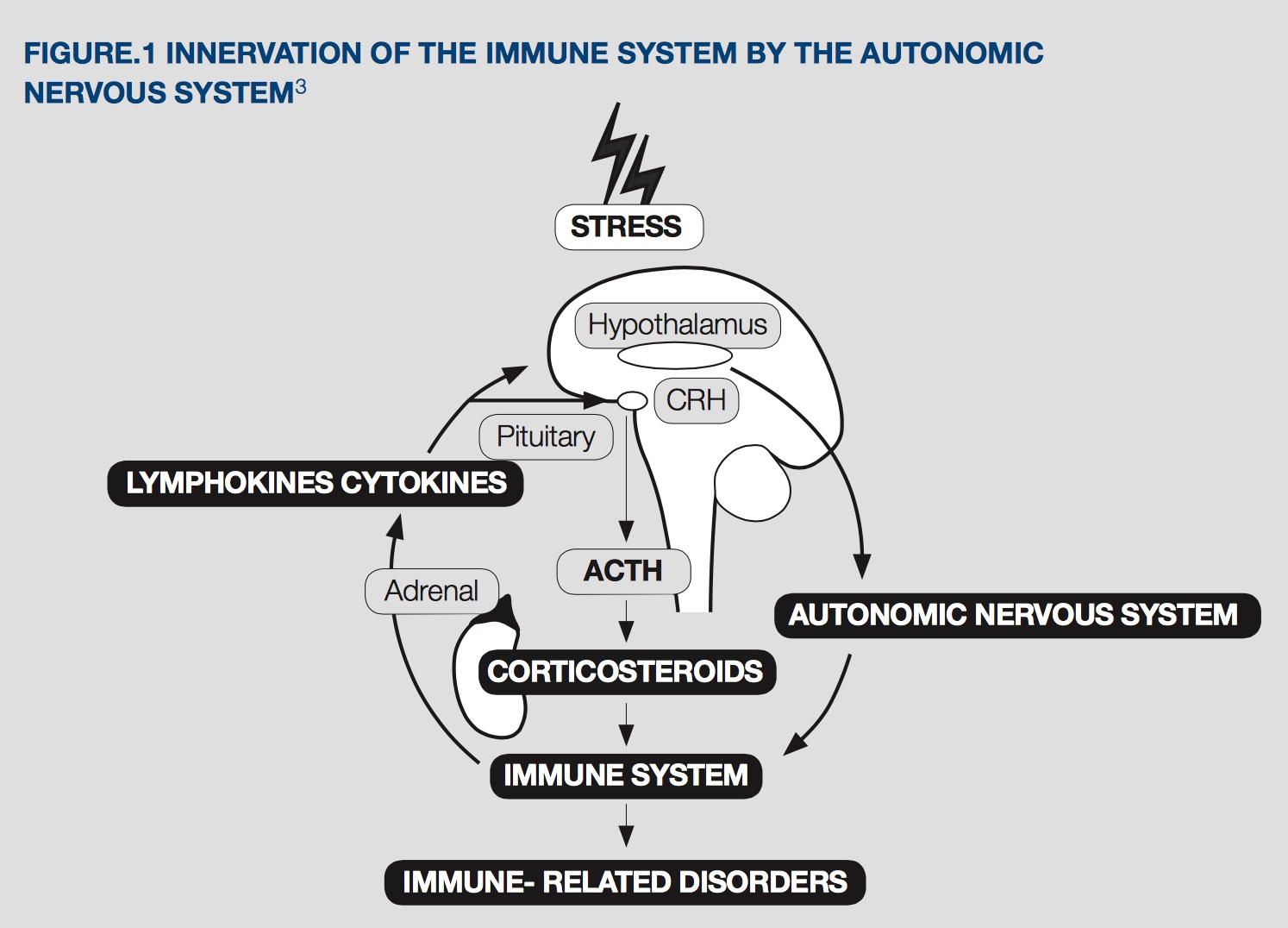
It is now known that the adrenal-immune relationship is even more intertwined, with bidirectional communication between the immune system and the hypothalamus-adrenal-pituitary (HPA) axis. Psychological or somatic stressors activate a cascade of events that profoundly affect the immune system, while the immune system influences the HPA axis to possibly modulate itself and prevent immune over-activation.[3]
The effect of stress on the HPA axis, adrenal function and immune health
Recent studies have confirmed that various chronic life stressors, such as bereavement, job-related stress, divorce or mental challenges (e.g. exams) inhibit immune function and increase susceptibility to infection through stress-induced increases in circulating glucocorticoid secretion.[3]
The increased release of cortisol, from the adrenal cortex, occurs through the stimulation of corticotrophin releasing factor (CRF) in the hypothalamus and, in turn, the release of adrenocorticotrophic hormone (ACTH) from the pituitary. When functioning normally, a negative feedback loop regulates the system so that when glucocorticoid levels are elevated, CRF and ACTH output is reduced.[4]
If there is prolonged or repeated stress, the adrenal gland’s ability to cope may falter, hippocampal atrophy and neuronal death can occur, and responsiveness to stressors diminishes. This results in accumulated tissue levels of cortisol and subsequent peripheral resistance, along with reduced circulating cortisol. This stage is called HPA resistance and, if continues, may lead to adrenal/HPA exhaustion.[5,6]
Table 1. Stages of the general adaptation syndrome (GAS)[6,23]
|
Stress response stage |
HPA reaction |
Result |
|
Stage 1 |
HPA activation/reaction |
↑cortisol, DHEA, adrenaline, noradrenaline |
|
Stage 2 |
HPA resistance |
↓cortisol, serotonin ↑ brain CRF, tissue cortisol and adrenaline (leads to peripheral resistance) |
|
Stage 3 |
HPA exhaustion |
↓CRF, ACTH, cortisol, may have ↓DHEA, serotonin, adrenaline and noradrenaline |
Glucocorticoid concentrations are also associated with immune activation by numerous antigens and can affect a number of cytokines. Therefore, glucocorticoids can stimulate the immune system to act against stressors. CRF and ACTH can also alter the immune system function directly – ACTH has a high binding affinity with lymphocytes, while CRF may modulate immunity by acting directly on splenocytes.[3]
Furthermore, chronic stress, with lowered circulating cortisol or a dysfunctional HPA axis, affects the immune system negatively through diminished cytokine and overall immune regulation. This can lead to disease, infections and increased inflammation.[3,5] As a result of the immune system being susceptible to glucocorticoid levels and through using the HPA axis to modulate its own activity, it is potentially vulnerable to both acute and chronic stress.[3]
Include Adrenal Support in Immune Protocols
Many of the nutrients and herbs used in adrenal formulas are not traditionally targeted at immune health. But with the physiological links and regulatory aspects connecting the stress response and the immune system, it would be beneficial to consider providing additional adrenal support during the winter months, especially in those prone to seasonal stress and infections, and anyone under physiological or psychological stress.
Herbal support
Adaptogens refer to a number of herbs that function to normalise stress levels, through the reduction of cortisol and other intracellular and extracellular mediators. Withania somnifera has been used in this role for over 300 years, reducing stress levels and increasing stamina and vitality.[7,8]
In addition to reducing salivary cortisol levels, withania has also been shown to modulate or mimic gamma-aminobutyric acid (GABA) and increase the androgenic hormone, dehydroepiandrosterone sulfate (DHEAS) production from the adrenal medulla, as it is often reduced in times of stress.[9,10]
When a high-concentration full-spectrum extract of withania KSM-66® was given to adults complaining of mental stress, it significantly reduced perceived stress levels by 44% and morning cortisol levels by 27.9%. Along with these reductions, the 600mg dose given for 60 days also had a significant impact upon overall stress, anxiety, insomnia, depression and social dysfunction scales.[11] This same extract reduced ‘comfort’ or emotional eating and food cravings, with improvements in body weight management of chronically stressed individuals.[9]
Magnolia officinalis and Phellodendron amurense, two herbs used in a registered combination called Relora®, have also been found to reduce salivary cortisol levels and increase DHEA. One study, using 500mg of Relora® each day, reduced the salivary cortisol levels by 18% after 4 weeks. This same research found the treatment group had significantly reduced perceived stress levels and improved mood parameters for tension, depression, anger fatigue and confusion.[12]
As a standardised formulation, Relora® contains 1.5% honokiol from magnolia and 0.1% berberine from phellodendron. These active ingredients work together to support the antistress and anti-anxiety benefits. Experimental studies also indicate that honokiol increases GABA receptor efficiency and production.[13,14]
Other examples of herbal support include, the adaptogenic herb Rhodiola rosea, the various ginsengs and the adrenal tonic Glycyrrhiza glabra.
Nutritional support
When looking at adrenal and immune health, vitamin C plays a crucial role in supporting both systems. The adrenal gland is one of the body’s organs with the highest level of vitamin C, but during stress these levels drop. Giving vitamin C supplementation appears to increase stress adaptation and normalise ACTH and cortisol levels. Vitamin C is also necessary for the conversion of dopamine to noradrenaline and the production of monoamine neurotransmitters, such as serotonin.[4,15]
Magnesium is an important mineral for adrenal function and is required for numerous metabolic pathways. When catecholamines and cortisol are increased, there is a shift of magnesium from the intracellular space to the extracellular space, potentially increasing urinary magnesium excretion. This reduction in intracellular magnesium then increases catecholamine production by the adrenals. Therefore, reduced magnesium intake or increased and prolonged stress, can increase a magnesium deficiency, result in a dysregulated HPA axis and lead to increased anxiety and stress.[16,17]
Additionally, magnesium is necessary for the conversion of vitamin B5 to coenzyme A (CoA) as well as for converting 5-hydroxytryptophan (5-HTP) to serotonin, and for GABA modulation.[4,16] There is also evidence suggesting magnesium as a potential immune modulator, with low magnesium levels promoting low-grade inflammation and increased C-reactive protein (CRP) levels.[18]
Another supportive nutrient, often overlooked for modulating stress, is phosphatidylserine (PS). PS is a type of phospholipid, an essential component of all biological membranes and is therefore crucial for cellular signalling, and enzymatic and cell receptor activity. As a phospholipid, PS may also have a modulatory role on the HPA axis, buffering chronic stress reactivity and restoring both ACTH and cortisol response in adrenal exhaustion. Studies have shown PS to impact ACTH and cortisol response under stressful stimuli.[19,20,21]
Comprising 15% of total brain phospholipids, PS has been studied in the area of cognitive performance after induced stress. In one randomised trial, 200mg of PS was given to male teenagers for 6 weeks. The subjects completed arithmetic tests at the beginning and end of the study period, with the results showing those taking the PS had similar academic results to the control group but with higher states of relaxation before and after testing. PS supplementation reduced the activation of specific front brain regions immediately after the tests, thereby inducing relaxation and decreasing stress.[19]
Other beneficial nutrients for adrenals include the amino acids tyrosine and glutamine, which can provide support in the production of catecholamines and dopamine as well as for glutathione production and GABA activity.[4,22]
Additionally, the B vitamins are critical for energy production and homeostasis, especially in the cooler months. Vitamin B5 has the added role of being essential for the production of CoA and therefore the production of the steroid hormones. While vitamin B6, as activated B6 pyridoxal-5-phosphate (P5P), is a central cofactor in the production of serotonin, dopamine and GABA. A deficiency in either of these vitamins can reduce adrenal function, with an inability to respond to stressful stimuli appropriately.[4,23,24]
The above herbs and nutrients indirectly support the immune system through their ability to reduce stress, improve adrenal function, produce important biological compounds and modulate the HPA axis. The regulatory action of the HPA axis on immune function, and the detrimental effects constant stress has on both the adrenals and the immune system, may be the key in treating stress and seasonal-related illness during the winter months.
References
- Mental Health First Aid Australia. Mental health training for the workplace - blended learning 2016. [Link]
- Australian Human Resources Institute. Absence management 2016. [Link]
- Nelson RJ, Demas GE, Klein SL, et al. Seasonal patterns of stress, immune function, and disease. New York: Cambridge University Press; 2002. [Link]
- Head K, Kelly G. Nutrients and botanicals for treatment of stress: Adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Altern Med Rev 2009;14(2):114-140. [Full Text]
- McEwen B. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharma 2000;22(2):108-124. [Full Text]
- Alschuler L. Optimizing the HPA axis. Naturopathic Doctor News & Review 2014;10(8):1-8. [Full Text]
- Panossian A. Adaptogens in mental and behavioral disorders. Psychiatr Clin North Am 2013;36(1):49-64. [Abstract]
- Dhar N, Razdan S, Rana S, et al. A decade of molecular understanding of withanolide biosynthesis and in vitro studies in Withania somnifera (L.) Dunal: Prospects and perspectives for pathway engineering. Frontiers in Plant Science 2015;6:1031.[Full Text]
- Choudhary D, Bhattacharyya S, Joshi K. Body weight management in adults under chronic stress through treatment with Ashwagandha root extract: A double-blind, randomized, placebo-controlled trial. J Evid Based Complementary Altern Med 2016; ePub ahead of print [Abstract]
- Auddy B, Hazra P, Mitra P. et al. A standardized Withania somnifera extract significantly reduces stress-related parameters in chronically stressed humans: A double-blind, randomized, placebo-controlled study. J Am Nutraceutical Assoc 2008;11:50-56. [Full Text]
- Chandrasekhar K, Kapoor J, Anishetty S. A prospective, randomized double-blind, placebo-controlled study of safety and efficacy of a high-concentration full-spectrum extract of Ashwagandha root in reducing stress and anxiety in adults. Indian J Psychol Med 2012;34(3):255-262. [Full Text]
- Talbott SM, Talbott JA, Pugh M. Effect of Magnolia officinalis and Phellodendron amurense (Relora(R)) on cortisol and psychological mood state in moderately stressed subjects. J Int Soc Sports Nutr 2013;10(1):37.[Full Text]
- Woodbury A, Yu SP, Wei L, et al. Neuro-modulating effects of honokiol: A review. Front Neurol 2013;4:130. [Full Text]
- Alexeev M, Grosenbaugh DK, Mott DD, et al. The natural products magnolol and honokiol are positive allosteric modulators of both synaptic and extra-synaptic GABA(A) receptors. Neuropharmacol 2012;62(8):2507-2514. [Full Text]
- Patak P, Willenberg HS, Bornstein SR. Vitamin C is an important cofactor for both adrenal cortex and adrenal medulla. Endocr Res 2004;30(4):871-875. [Abstract]
- Sartori SB, Whittle N, Hetzenauer A, et al. Magnesium deficiency induces anxiety and HPA axis dysregulation: Modulation by therapeutic drug treatment. Neuropharmacol 2012;62(1):304-312. [Full Text]
- Seelig MS. Consequences of magnesium deficiency on the enhancement of stress reactions; preventive and therapeutic implications (a review). J Am Coll Nutr 1994;13(5):429-446. [Abstract]
- Brilla LR. Magnesium influence on stress and immune function in exercise. J Sports Med Doping Studies 2012;02(03). [Full Text]
- Baumeister J, Barthel T, Geiss KR, et al. Influence of phosphatidylserine on cognitive performance and cortical activity after induced stress. Nutr Neurosci 2008;11(3):103-110. [Abstract]
- Hellhammer J, Vogt D, Franz N, et al. A soy-based phosphatidylserine/ phosphatidic acid complex (PAS) normalizes the stress reactivity of hypothalamus-pituitary-adrenal-axis in chronically stressed male subjects: A randomized, placebo-controlled study. Lipids Health Dis 2014;13:121. [Full Text]
- Starks MA, Starks SL, Kingsley M, et al. The effects of phosphatidylserine on endocrine response to moderate intensity exercise. J Int Soc Sports Nutr 2008;5:11. [Full Text]
- Walls AB, Waagepetersen HS, Bak LK, et al. The glutamine-glutamate/GABA cycle: Function, regional differences in glutamate and GABA production and effects of interference with GABA metabolism. Neurochem Res 2015;40(2):402-409. [Abstract]
- Anderson DC. Assessment and nutraceutical management of stress-induced adrenal dysfunction. Integrat Med: A Clinic J 2008;7(5):18-25. [Full Text]
- Kelly GS. Pantothenic acid monograph. Altern Med Rev 2011;16(3):263-274. [Full Text]
- Casey L. Stress and wellbeing in Australia survey 2013. Australian psychological society: Melbourne. [Link]
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.


