Pre-menstrual Dysphoric Disorder (PMDD) is a severe type of premenstrual syndrome. It is characterised by moderate to severe affective and behavioural symptoms that occur post ovulation and peak in the luteal phase of the menstrual cycle, becoming minimal or absent at the onset of menstruation.1 PMDD is believed to affect 3-8%2 of women worldwide.
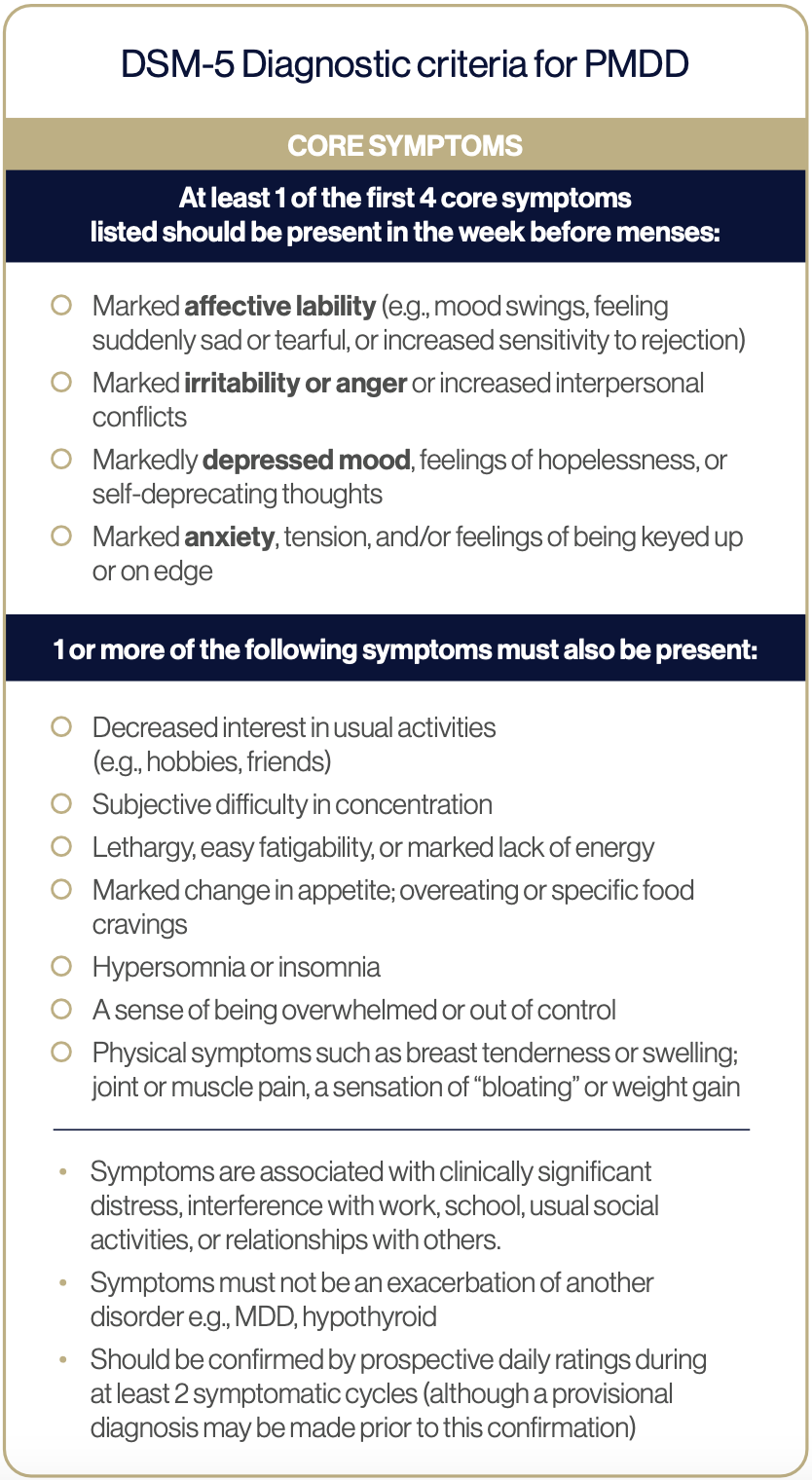
Diagnostic criteria
In 2022, PMDD was added to the International Classification of Diseases 11th Revision (ICD-11) and placed under the category of gynaecological diseases.3 PMDD is also listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) as a separate entity under depressive disorders.
Pathophysiology
Hormones such as pregnenolone, progesterone, oestradiol, and corticosterone can be synthesised in the brain where they function as neuro-active steroids (NAS’s).5 Here they act on neuron receptors in parts of the brain that influence mood, cognition and behaviour, influencing the release of neurotransmitters (NT’s) such as serotonin, GABA and dopamine.6 Symptoms of PMDD are partially driven by central nervous system sensitivity to normal fluctuations in neuroactive steroid hormones (NASs) and their subsequent action on NT’s.7
Allopregnanolone
A sensitivity to rising levels of progesterone in the luteal phase and its metabolite, allopregnanolone (ALLO) have been implicated in the pathogenesis of PMDD.8 In women without PMDD, modulation of the GABA-a receptor by ALLO results in reduced anxiety and mild sedation. Paradoxically women with PMDD show altered GABA-a receptor sensitivity to rising levels of ALLO, resulting in mood and behavioural disturbances such as aggression, anxiety and poor executive function.9,10
Serotonin
Women with PMDD demonstrate altered serotonergic activity in the luteal phase of the menstrual cycle. This is largely driven by withdrawal of oestrodiol. Oestrodiol is known to increase serotonergic activity via multiple mechanisms including:
- increasing serotonin transporter mRNA, particularly in brain areas involved with emotion and behaviour,11
- increasing production of tryptophan hydroxylase, the enzyme responsible for the conversion of tryptophan to serotonin.12
Melatonin
Plasma melatonin has been shown to be delayed in the luteal phase of women with PMDD and is believed to contribute to mood disturbances. This may be due to blunted serotonin production, the latter of which is a precursor for melatonin production.
AETIOLOGY
Genetics
Twin studies support a link between genetics and an increasing susceptibility for the development of PMDD. Polymorphisms are observed in many genes, including those coding for:13
- Serotonergic 5HT1A receptor
- Oestrogen 1 receptor alpha gene (ESR-1)
- ESC/E(Z).14
Trauma
Women who have a history of trauma are significantly more likely to experience PMDD than controls. An Australian study observed 83% of women with PMDD had experienced early life trauma, with emotional abuse being the most prevalent.15 While the underlying mechanisms are multifaceted, dysfunctional HPA- axis activity and subsequent altered neurotransmission may be responsible.16
Chronic stress
Women with PMDD demonstrate a maladaptive response to stressors highlighted by a flattened diurnal cortisol slope,17 thus suggestive of HPA axis dysfunction. This may explain their perception of daily events as more stressful and their higher arousal of negative feelings in the luteal phase of the cycle. Chronic stress alters the composition of GABA-a receptors reducing tonicity,18 which may partly explain the paradoxical reaction to rising levels of ALLO, and subsequent heightened stress reactivity.
Comorbidities
\Women with PMDD should be considered a high-risk group for suicidality. Meta-analysis of thirteen studies demonstrates that PMDD patients were at an almost seven times higher risk of suicide attempt.19 Practitioners awareness of working in conjunction with a mental health professional needs to be highlighted to ensure optimal patient care. Women with bipolar 20,21 and ADHD 22 also demonstrate a higher prevalence of PMDD.
SUPPLEMENTATION
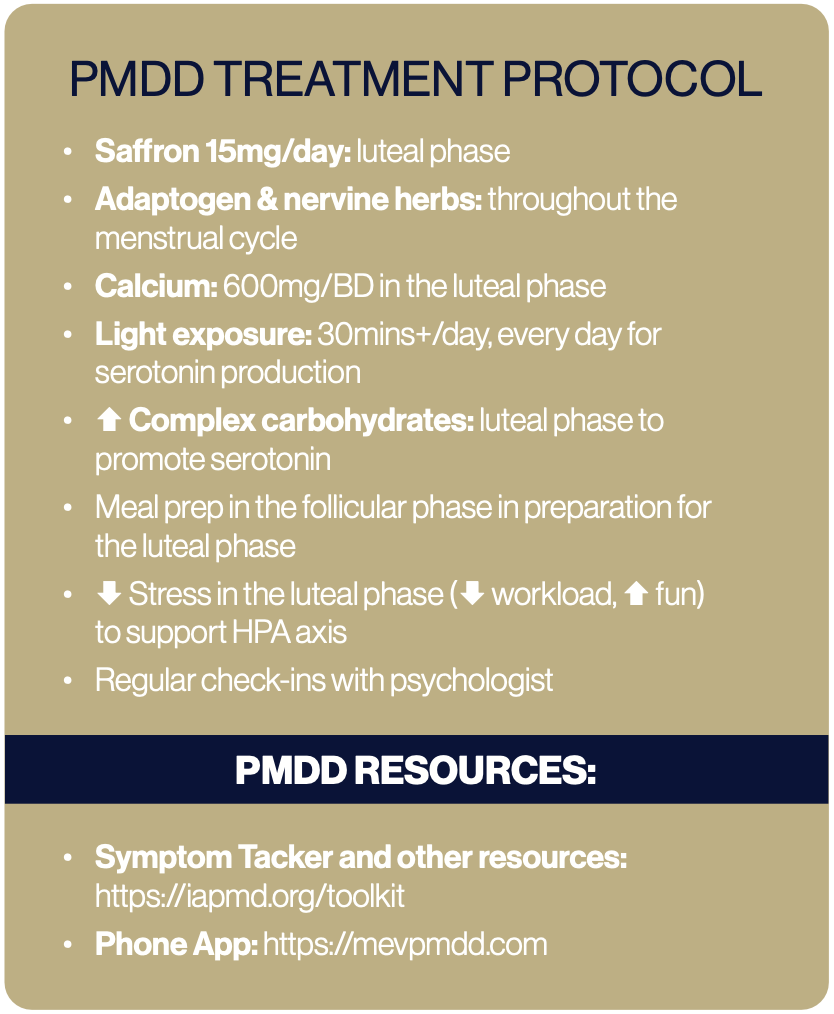
Calcium 600mg/twice daily 23 (luteal phase)
Alterations in cyclical calcium homeostasis have been observed in women with PMDD compared to healthy controls.24 Calcium channels are involved with the release of monoamines including serotonin and dopamine, it is hypothesised that dysregulated levels of calcium in the luteal phase may drive neuronal dysfunction. Feelings of irritability, depression, anxiety, and mania experienced by individuals with PMDD are enhanced. Oestrodiol has a regulating action on calciotropic hormones, thus withdrawal of oestrodiol will influence cellular calcium concentrations.25 It is interesting to note that many of the mood symptoms associated with low calcium mimic that of PMDD.
Myo-inositol 2g/day (luteal phase)
Myo-inositol may be useful for the management of PMDD due to its role as a second messenger of serotonin, however contradictory results have been seen. An early 2002 study using a high dose of myo-inositol (12g/day) taken in the luteal phase of the cycle showed no efficacy compared to placebo.26 However a later study utilising a lower dose of 2g/day of myo- inositol consumed over 6 menstrual cycles was associated with a statistically significant improvement in the Hamilton Depression Rating scale and the Clinical Global Impression-Severity of Illness scale in women with PMDD.27
HERBAL
Crocus sativus (Saffron)
Supplementation with Crocus sativus (15mg twice daily) over two menstrual cycles has been shown to assist with improving mood in individuals with PMDD.28 The active constituents, crocin and safranal found with in Crocus sativus are believed to inhibit the reuptake of dopamine, norepinephrine and serotonin, contributing to its mood enhancing effects.
Adaptogen & Nervine herbal medicines
Due to the HPA axis dysfunction observed in women with PMDD, herbal medicines with adaptogen and nervine actions may be useful, though no studies have been conducted. Examples include Withania somnifera, Chamomila recutita, Centella asiatica and Rhodiola rosea (caution with anti-depressants).
NUTRITION
PMDD is associated with extreme cravings, driven by withdrawal of oestrodiol and serotonin. Women with PMDD should be encouraged to consume adequate whole food carbohydrates. Complex carbohydrates in the luteal phase assist with improving mood symptoms including depression, tension and anger by increasing brain synthesis of serotonin.29,30
LIFESTYLE
Light therapy
Light therapy is effective in enhancing mood in a range of mental health conditions, including PMDD. While exposure to sunlight is ideal, use of a light box may also be helpful. Thirty minutes of evening light therapy, administered via a light box in the luteal phase of the menstrual cycle, to women with PMDD has been shown to reduce premenstrual depression and tension scores.31
Download a PDF version of this article:
References
1 Tiranini L, Nappi RE. Recent advances in understanding/management of premenstrual dysphoric disorder/premenstrual syndrome. Fac Rev. 2022 Apr 28;11:11
2 Mishra S, Elliott H, Marwaha R. Premenstrual Dysphoric Disorder. 2023 Feb 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30335340 https://pubmed.ncbi.nlm.nih.gov/30335340/
3 Schroll JB, Lauritsen MP. Premenstrual dysphoric disorder: A controversial new diagnosis. Acta Obstet Gynecol Scand. 2022 101(5):482-483
4 Mishra S, Elliott H, Marwaha R. Premenstrual Dysphoric Disorder. 2023 Feb 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30335340 https://www.ncbi.nlm.nih.gov/books/NBK532307/
5 Szpunar MJ, Freeman MP. Investigational Treatment of Depressive Disorders With Neuroactive Steroids: Potential Implications for Premenstrual Dysphoric Disorder. J Clin Psychiatry. 2021 8;82(4):20ac13853
6 Hantsoo L, Epperson CN. Allopregnanolone in premenstrual dysphoric disorder (PMDD): Evidence for dysregulated sensitivity to GABA-A receptor modulating neuroactive steroids across the menstrual cycle. Neurobiol Stress.2020 4;12:100213.
7 Hantsoo L, Payne JL. Towards understanding the biology of premenstrual dysphoric disorder: From genes to GABA. Neurosci Biobehav Rev. 2023 Apr 12;149:105168
8 Carlini SV et al. Management of Premenstrual Dysphoric Disorder: A Scoping Review. Int J Womens Health. 2022 Dec 21;14:1783-1801
9 Bäckström T, et al. A randomized, double-blind study on efficacy and safety of sepranolone in premenstrual dysphoric disorder. Psychoneuroendocrinology. 2021 Nov;133:105426.
10 Bäckström T, et al. GABAA Receptor-Modulating Steroids in Relation to Women’s Behavioral Health. Curr Psychiatry Rep. 2015 Nov;17(11):92
11 Hantsoo L, Epperson CN. Premenstrual Dysphoric Disorder: Epidemiology and Treatment. Curr Psychiatry Rep. 2015 Nov;17(11):87
12 Itriyeva K. Premenstrual syndrome and premenstrual dysphoric disorder in adolescents. Curr Probl Pediatr Adolesc Health Care. 2022 May;52(5):101187
13 Hantsoo L, Epperson CN. Premenstrual Dysphoric Disorder: Epidemiology and Treatment. Curr Psychiatry Rep. 2015 Nov;17(11):87
14 Dubey N, et al. The ESC/E(Z) complex, an effector of response to ovarian steroids, manifests an intrinsic difference in cells from women with premenstrual dysphoric disorder. Mol Psychiatry. 2017 Aug;22(8):1172-1184.
15 Kulkarni J, et al. The prevalence of early life trauma in premenstrual dysphoric disorder (PMDD). Psychiatry Res. 2022 Feb;308:114381
16 Girdler SS, et al. Persistent alterations in biological profiles in women with abuse histories: influence of premenstrual dysphoric disorder. Health Psychol. 2007 Mar;26(2):201-13
17 Beddig T, et al. Stress, mood, and cortisol during daily life in women with Premenstrual Dysphoric Disorder (PMDD). Psychoneuroendocrinology. 2019 Nov;109:104372.
18 Jie F, et al. Stress in Regulation of GABA Amygdala System and Relevance to Neuropsychiatric Diseases. Front Neurosci. 2018 Aug 14;12:562
19 Prasad D, et al. Suicidal Risk in Women with Premenstrual Syndrome and Premenstrual Dysphoric Disorder: A Systematic Review and Meta-Analysis. J Womens Health (Larchmt). 2021 Dec;30(12):1693-1707
20 Sharma V, et al. Relationship of Premenstrual Dysphoric Disorder With Bipolar Disorder: A Systematic Review. J Clin Psychiatry. 2022 Oct 26;83(6):22r14416
21 Pearlstein T. Bipolar Disorder and Premenstrual Dysphoric Disorder: Comorbidity Conundrum. J Clin Psychiatry. 2022 Oct 26;83(6):22com14573.
22 Dorani F, et al. Prevalence of hormone-related mood disorder symptoms in women with ADHD. J Psychiatr Res. 2021 Jan;133:10-15 23 Lanza di Scalea T, Pearlstein T. Premenstrual Dysphoric Disorder. Med Clin North Am. 2019 Jul;103(4):613-628
24 Thys-Jacobs S, et al. Cyclical changes in calcium metabolism across the menstrual cycle in women with premenstrual dysphoric disorder. J Clin Endocrinol Metab. 2007 Aug;92(8):2952-9.
25 Arab A, et al. Beneficial Role of Calcium in Premenstrual Syndrome: A Systematic Review of Current Literature. Int J Prev Med. 2020 Sep 22;11:156
26 Nemets B, et al. Myo-inositol has no beneficial effect on premenstrual dysphoric disorder. World J Biol Psychiatry. 2002 Jul;3(3):147-9
27 Gianfranco C, et al. Myo-inositol in the treatment of premenstrual dysphoric disorder. Hum Psychopharmacol. 2011 Oct;26(7):526-30.
28 Rajabi F, et al. Saffron for the Management of Premenstrual Dysphoric Disorder: A Randomized Controlled Trial. Adv Biomed Res. 2020 Oct 30;9:60. d
29 Wurtman JJ, et al. Effect of nutrient intake on premenstrual depression. Am J Obstet Gynecol. 1989 Nov;161(5):1228-34
30 Lanza di Scalea T, Pearlstein T. Premenstrual Dysphoric Disorder. Med Clin North Am. 2019 Jul;103(4):613-628
31 Lam RW, et al. A controlled study of light therapy in women with late luteal phase dysphoric disorder. Psychiatry Res. 1999 Jun 30;86(3):185-92.
32 Parry BL, et al. A 1-week sleep and light intervention improves mood in premenstrual dysphoric disorder in association with shifting melatonin offset time earlier. Arch Womens Ment Health. 2023 Feb;26(1):29-37