Sleep is a physiological process that is essential for well-being and imperative for immune health. Despite the importance of sleep, many Australians experience sleep disturbances; with sleep disorders estimated to affect approximately 33-45 per cent of the Australian adult population.1
Although sleep is typically characterised by long periods of immobility, the immune system is highly active during this time, working to enhance immune defences through the promotion of innate and adaptive immunity. Unsurprisingly, host immunity to pathogens is greatly influenced by the lack of sleep. Interestingly however, this relationship is not one-sided.
“An activated immune system that is responding to a pathogen influences sleep quality and quantity, highlighting the bi-directional relationship that exists between sleep and immunity.”
The connection between immunity and sleep
Interleukin-6 (IL-6) is an important pleiotropic cytokine, that significantly increases in production during nocturnal hours, alongside an increase in REM sleep, highlighting its role as a putative ‘sleep factor’2. IL-6 exerts specific immune activity via multiple factors not limited to its effects on T cell regulation and the promotion of macrophage phagocytic activities.3 Early night sleep deprivation as well as total sleep deprivation are associated with the delayed release of IL-6, suggesting immune suppressive effects of total lack of sleep while also emphasising the importance of sleep timing on immune function.
The process of sleep is instrumental in facilitating the movement of immune cells to specific lymphatic tissues. Circulating immune cells, including undifferentiated naïve T cells, peak early in the night and subsequently decline throughout the nocturnal hours where they then move out of circulation into lymphoid organs.4 Being awake in the early hours of the night impedes this process, increasing susceptibility to infection.
Sleep supports the consolidation phase of immunological memory formation. During slow wave sleep, there is a transfer of antigenic information from antigen presenting cells to T cells, assisting the immune system to form a targeted immune response should it encounter a familiar antigen again.5
General recommendations around sleep quantity for optimal well-being and immune health suggest seven or more hours per night for healthy adults.6 Population studies however, demonstrate an increasing prevalence of adults sleeping less than 6 hours per night.7 This is hypothesised to be due to work and societal pressures (e.g., shift work and social jet lag where a person’s social commitments interfere with their biological chronotype), increased night-time light exposure due to smart phone addiction and poor dietary choices, for example increased intake of alcohol and caffeine - both of which are known to impact sleep quality and duration.
Risks of sleep deprivation
The consistent lack of sleep is associated with an increase in pro-inflammatory cytokines receptors release, including TNF-alpha, and a decrease in both anti-inflammatory cytokines receptors and natural killer activity.8 It is therefore no surprise that the lack of sleep is associated with an increased risk of infection. Individuals with habitually short sleep duration (<5 hours) are at increased risk of respiratory tract infections compared to those maintaining 7-8 hours of sleep.9 Inadequate sleep may also influence viral reactivation, with a 1.23-fold increase in the reactivation of latent herpes zoster virus observed in individuals with a sleep disorder.10 Immunised people after four consecutive nights of sleep restricted to just 4 hours were found to have IgG antibody titres 50% lower than individuals who had slept adequately, demonstrating a reduction in vaccine efficacy in people experiencing sleep deprivation.11
Risk of infection to sleep
While sleep clearly influences overall immune function, immunological challenges such as viral or bacterial infection can alter normal sleep patterns. Infection is associated with dramatic alterations in sleep quality and quantity, namely greater time in slow sleep wave and consequently decreased REM sleep.12 This is in part due to the direct action from the pathogen, for example the release of viral peptides potentially infecting the central nervous system, but also due to an adaptive homeostatic response utilised by the host to divert energy to the immune system to eliminate the infection.
Sleep is an important modulator of immunity that can enhance immune defence, however, healthy sleep requires appropriate duration, quality, timing, and regularity. Given the interconnectedness of sleep and circadian rhythms, it is also imperative to understand and modify circadian disruption to support immunity.
References
[1] Adams, RJ., Appleton, SL., Taylor, AW., Gill, TK., Lang, C., McEvoy, RD., & Antic, NA. Sleep health of Australian adults in 2016: Results of the 2016 Sleep Health Foundation national survey. Sleep Health. 2017 3(1), 35–42.
[2] Vgontzas AN, Bixler EO, Lin HM, Prolo P, Trakada G, Chrousos GP. IL-6 and its circadian secretion in humans. Neuroimmunomodulation. 2005;12(3):131-40.
[3] Velazquez-Salinas L, Verdugo-Rodriguez A, Rodriguez LL, Borca MV. The Role of Interleukin 6 During Viral Infections. Front Microbiol. 2019 May 10;10:1057.
[4] Besedovsky L, Lange T, Haack M. The Sleep-Immune Crosstalk in Health and Disease. Physiol Rev. 2019 Jul 1;99(3):1325-1380
[5] Besedovsky L, Lange T, Haack M. The Sleep-Immune Crosstalk in Health and Disease. Physiol Rev. 2019 Jul 1;99(3):1325-1380.
[6] Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015 Jun 1;38(6):843-4.
[7] Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. 2021 Nov 18;4(1):1304.
[8] Silva ESME, Ono BHVS, Souza JC. Sleep and immunity in times of COVID-19. Rev Assoc Med Bras (1992). 2020 Sep 21;Suppl 2):143-147.
[9] Prather AA, Leung CW. Association of Insufficient Sleep With Respiratory Infection Among Adults in the United States. JAMA Intern Med 2016, 176: 850–852
[10] Chung WS, Lin HH, Cheng NC. The Incidence and Risk of Herpes Zoster in Patients With Sleep Disorders: A Population-Based Cohort Study. Medicine (Baltimore). 2016 Mar;95(11):e2195.
[11] Benedict, C., & Cedernaes, J. Could a good night's sleep improve COVID-19 vaccine efficacy?. The Lancet. Respiratory medicine, 2021 9(5), 447–448.
[12] Ibarra-Coronado EG, Pantaleón-Martínez AM, Velazquéz-Moctezuma J, Prospéro-García O, Méndez-Díaz M, Pérez-Tapia M, Pavón L, Morales-Montor J. The Bidirectional Relationship between Sleep and Immunity against Infections. J Immunol Res.2015:678164.
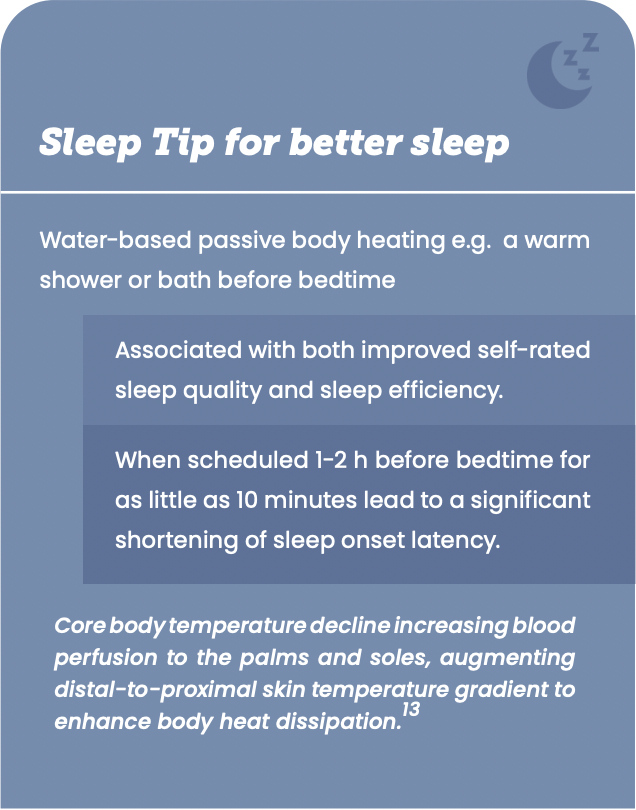
[13] Haghayegh S, Khoshnevis S, Smolensky MH, Diller KR, Castriotta RJ. Before-bedtime passive body heating by warm shower or bath to improve sleep: A systematic review and meta-analysis. Sleep Med Rev. 2019 Aug;46:124-135.
Download a free PDF copy of this article
This image by FX Medicine is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
More information about how to share/use this download for personal use.
If you interested in using any FX Medicine content for commercial use please contact us.
DISCLAIMER:
The information provided on FX Medicine is for educational and informational purposes only. The information provided on this site is not, nor is it intended to be, a substitute for professional advice or care. Please seek the advice of a qualified health care professional in the event something you have read here raises questions or concerns regarding your health.