Chronic pain affects 20% of people. Approximately 50% of adults report having pain in the previous 3 months, with 11% reporting daily experiences of pain.1,2 In a significant portion of chronic pain cases, however, definitive peripheral causes of chronic pain cannot be identified. Many people reporting severe pain do not have objective markers consistent with the report of pain.3,4 For example, over 80% of people with chronic back pain reveal no evidence of objective pathology. These findings indicate that other factors are at play apart from medical.
The biopsychosocial approach purports pain and pain-related behaviour results from an interplay among biological, psychological, social, and contextual factors.5-7 Everyone has a unique genotype and life history, varying life circumstances, worries, and stresses. These dimensions interact influencing a person’s response to chronic pain.
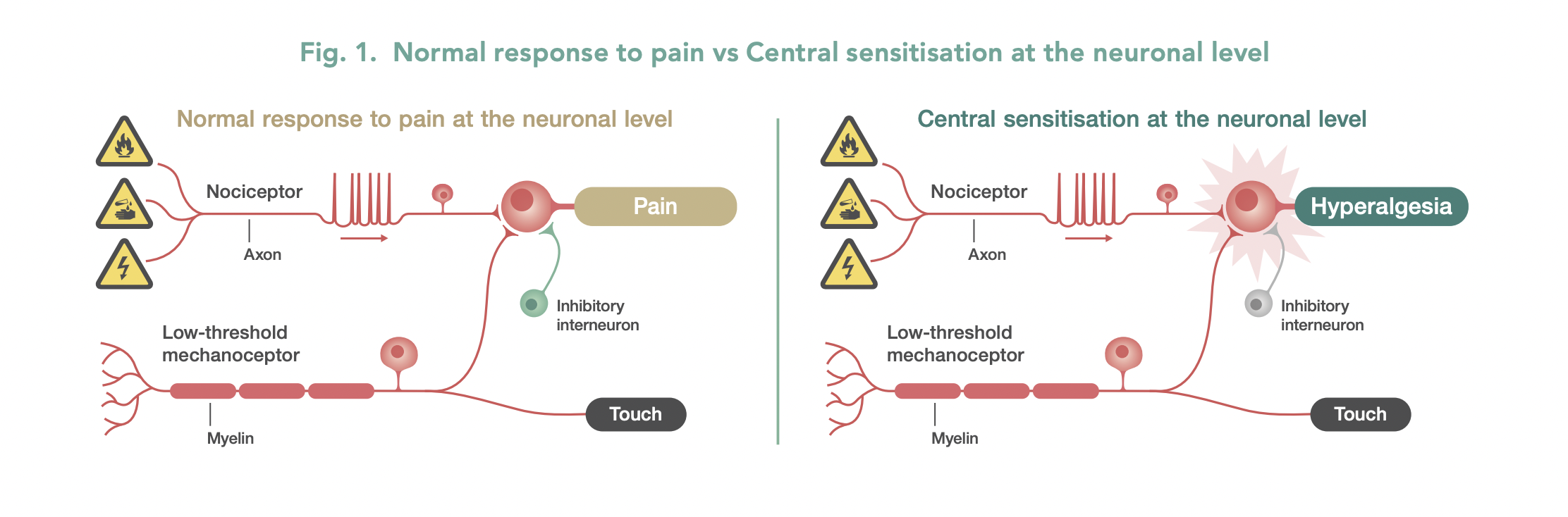
Central sensitivity syndrome (CSS) is an increased response of the pain neurons (nociceptive) in the central nervous system to sensory stimuli.5 (See Figure 1). A significant portion of people with chronic pain, including those suffering from fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, chronic pelvic pain, temporomandibular joint disorder, and migraine experience CSS.5,8,9 In CSS, the peripheral nerves function normally, however the functioning of neurons in the spinal cord and brain is affected.
Central Sensitivity Syndrome patients experience heightened pain sensitivity and pain diffusion, along with lowered pain thresholds.
Factors affecting central sensitivity
Central sensitivity is influenced by biological, psychological, and social factors.5 (See Figure 2).
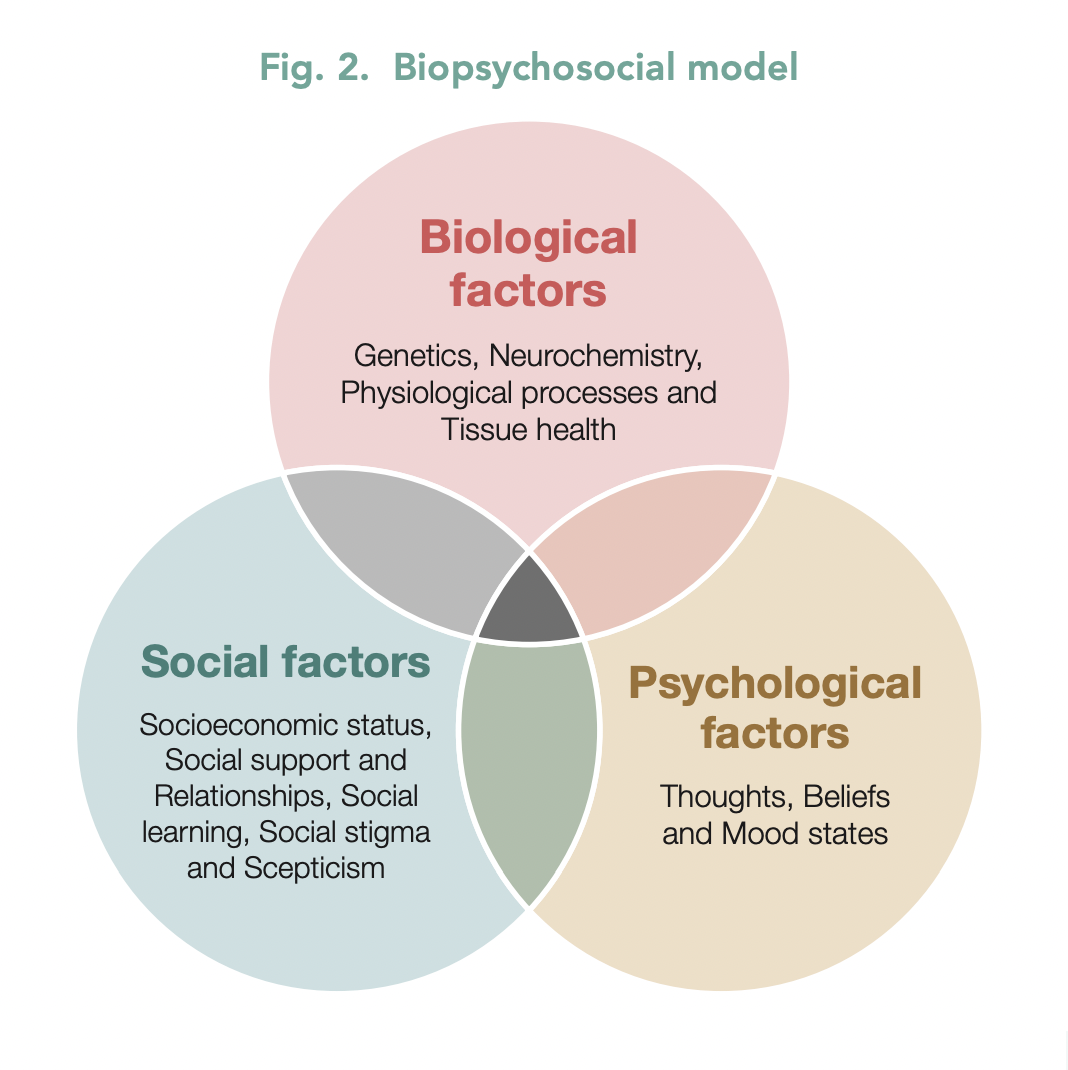
Biological factors: include genetics, neurochemistry, physiological processes and tissue health.
Psychological factors: include the patient’s thoughts, beliefs and mood states. Self-efficacy around pain refers to a person’s confidence in their ability to manage pain; research shows low pain self-efficacy is associated with increased pain perception.10
Pain-catastrophic thinking occurs when people dwell on the worst possible outcomes; again associated with increased pain perception and disability.11 Pain catastrophisers magnify difficulties associated with their pain, constantly obsess about the pain, and have an increased sense of helplessness. There exists a bi-directional relationship between mood and pain.
Depression or an anxiety disorder increases the risk of suffering from chronic pain. Depression exacerbates mental health disorders and pain-related treatment outcomes.
A patient’s history impacts these psychological factors. Childhood maltreatment and past traumas affect mood, beliefs and thoughts. Research confirms past trauma is associated with increased pain sensitivity and an increased risk of suffering from chronic pain.12,13
Social factors: affecting central sensitivity include socioeconomic status, social support and relationships, social stigma and scepticism, and social learning. Being around others with stigmatising attitudes toward pain or scepticism increases pain severity and disability. Alternatively, those given positive social support generally have a better prognosis.14 The attitudes of family, partners, friends and health professionals are important in a person’s pain recovery.
Changes in diet, lifestyle behaviours, sleep quality, and appropriate nutraceutical and phytoceutical supplementation also impact the best outcomes for our patients.
The biopsychosocial approach forms an integral part of the psychological treatment of pain. Cognitivebehaviour therapy and other psychological treatments for pain attempt to modify people’s thoughts, beliefs, and behaviours that contribute to increased pain sensitivity, reduce overall quality of life, and negatively impact social, psychological, and occupational functioning. Pain psychology is not about minimising pain and denying its existence. The pain sensation is real, but the biopsychosocial factors that can affect pain must be considered to optimise treatment.
Pain Reprocessing Therapy: rewiring neural pathways
Psychological approaches have regularly demonstrated effective pain reduction and suffering, improved mood, and overall quality of life.15-17 A recent treatment, the ‘Pain Reprocessing Therapy’ was provided to patients with chronic back pain. After 4 weeks, 66% of participants were pain-free or nearly pain-free, as compared to 20% randomised to a placebo intervention and 10% randomised to usual care. These gains were largely maintained at a one-year follow-up.18
Download a PDF version of this article
References
1. Dahlhamer, J., et al., Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults - United States, 2016. MMWR Morb Mortal Wkly Rep, 2018. 67(36): p. 1001-1006.
2. Nahin, R.L., Estimates of pain prevalence and severity in adults: United States, 2012. J Pain, 2015. 16(8): p. 769-80.
3. Deyo, R.A., Early diagnostic evaluation of low back pain. J Gen Intern Med, 1986. 1(5): p. 328-38.
4. Maher, C., M. Underwood, and R. Buchbinder, Non-specific low back pain. Lancet, 2017. 389(10070): p. 736-747.
5. Adams, L.H., Turk, D.C., Central sensitization and the biopsychosocial approach to understanding pain. J Appl Behav Res, 2018. 23(2): p. 1-18.
6. Meints, S.M. and R.R. Edwards, Evaluating psychosocial contributions to chronic pain outcomes. Prog Neuropsychopharmacol Biol Psychiatry, 2018. 87(Pt B): p. 168-182.
7. Till, S.R., S. As-Sanie, and A. Schrepf, Psychology of Chronic Pelvic Pain: Prevalence, Neurobiological Vulnerabilities, and Treatment. Clin Obstet Gynecol, 2019. 62(1): p. 22-36.
8. Fleming, K.C. and M.M. Volcheck, Central sensitization syndrome and the initial evaluation of a patient with fibromyalgia: a review. Rambam Maimonides Med J, 2015. 6(2): p. e0020.
9. Midenfjord, I., et al., Central sensitization and severity of gastrointestinal symptoms in irritable bowel syndrome, chronic pain syndromes, and inflammatory bowel disease. Neurogastroenterol Motil, 2021. 33(12): p. e14156.
10. Raman, S., Sharma, P., Self-efficacy as a mediator of the relationship between pain and disability in chronic pain patients: a narrative review. Bulletin of Faculty of Physical Therapy, 2022.
11. Petrini, L. and L. Arendt-Nielsen, Understanding Pain Catastrophizing: Putting Pieces Together. Front Psychol, 2020. 11: p. 603420.
12. Maatta, J., et al., High Level of Childhood Trauma Predicts a Poor Response to Spinal Cord Stimulation in Chronic Neuropathic Pain. Pain Physician, 2019. 22(1): p. E37-E44.
13. Lumley, M.A., et al., Trauma matters: psychological interventions for comorbid psychosocial trauma and chronic pain. Pain, 2022. 163(4): p. 599-603.
14. Wilson, J.M., et al., Social Support and Psychological Distress among Chronic Pain Patients: The Mediating Role of Mindfulness. Pers Individ Dif, 2022. 190.
15. Ho, E., et al., Psychological interventions for chronic non-specific low back pain: protocol of a systematic review with network meta-analysis. BMJ Open, 2020. 10(9): p. e034996.
16. McCracken, L.M., L. Yu, and K.E. Vowles, New generation psychological treatments in chronic pain. BMJ, 2022. 376: p. e057212.
17. Braunwalder, C., et al., Are Positive Psychology Interventions Efficacious in Chronic Pain Treatment? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Med, 2022. 23(1): p. 122-136.
18. Ashar, Y.K., et al., Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial. JAMA Psychiatry, 2022. 79(1): p. 13-23